(older posts in this series follow on at the bottom - pls. scroll down)
 It was a busy week in Stockholm, Sweden for the annual meeting of the International Society for Stem Cell Research. A great choice of city and so calm for a capital - beauty, innovation and peace! The schedule was somewhat of a juggling act to manage as science sessions, meetings, interviews, posters & exhibitors needed to be balanced. Sadly I wasn't able to explore fully the great selection of Exhibitors, nor attend all my earmarked science sessions, as I would have liked due to time limitations. Also off-site socials were limited to members only, so I missed some cocktail get togethers which would have been fun! A good iPad agenda tool by ISSCR, which I used constantly, made life a lot easier. Thx for that!
It was a busy week in Stockholm, Sweden for the annual meeting of the International Society for Stem Cell Research. A great choice of city and so calm for a capital - beauty, innovation and peace! The schedule was somewhat of a juggling act to manage as science sessions, meetings, interviews, posters & exhibitors needed to be balanced. Sadly I wasn't able to explore fully the great selection of Exhibitors, nor attend all my earmarked science sessions, as I would have liked due to time limitations. Also off-site socials were limited to members only, so I missed some cocktail get togethers which would have been fun! A good iPad agenda tool by ISSCR, which I used constantly, made life a lot easier. Thx for that!
Tuesday evening's pre-meeting public science session kicked off the event for me, which was focused on the Aging Brain, off-site at Karolinska Institute with 4 great speakers. The overall event ran, as many know, through Saturday early evening with the closing presentations.
Over the next few days I will be doing some review pieces on the event and some highlights. In addition, there are a number of more in-depth pieces I will feature in-time with material from the interviews I conducted. All in all a great show and thx to the organizers for their best-in-class effort.
Stay tuned...
Cheers
Ref: Interviews (i) / post-presentation Chats (c) / Meetings (m) / Exhibitor Briefing (eb) / Poster Review (pr) held with:
Austin Smith (i)
Jeanne Loring (i)
Robin Ali (i)
Masayo Takahashi (i)
Rudolf Jaenisch (i)
Sally Temple (i)
Robert Langer (i)
Malin Parmar (c)
Hans Keirstead (c)
Jonathan Thomas (m)
Derek van der Kooy (m)
Tim Caulfield (m)
ESI Bio (eb)
Corning (eb)
Miltenyi Biotec (eb)
UCL (eye - pr)
Whitehead Institute (direct diff/eye - pr)
Riken (eye - pr)
Iserm (eye - pr)
Karolinska (eye - pr)
Neural SCI (eye - pr)
CHA (eye - rep no-show - pr)
Ocata/Cha (eye - rep no-show - pr)
U.Toronto (eye - pr)
U.Pitt (eye - pr)
U.Finland (eye - pr)
U. Taiwan (eggs - pr)
_________________________________________________________________
Stem Cells & The Aging Brain
Public Symposium @ Karolinska Institute - Pre-Meeting Event

 One of the best aspects of going to a new city is exploring, which I had a little time to do on Tuesday before the official start of events. Stockholm has always been on my list but until last week had slipped through undiscovered. All the more reason to attend ISSCR’s annual event! I believe a few of the attendees also felt that was a good hook...
One of the best aspects of going to a new city is exploring, which I had a little time to do on Tuesday before the official start of events. Stockholm has always been on my list but until last week had slipped through undiscovered. All the more reason to attend ISSCR’s annual event! I believe a few of the attendees also felt that was a good hook...
 The old city is a magical labyrinth of cobblestone and majestic buildings - rising higher than I thought would be the case. Each seeking out the light and colored in different facade hues. Of course any city centre is filled with tourist shops, but for some reason Stockholm’s heart doesn't seem overly commercial. Above all it’s the ambience of sophisticated posture and calm that permeates the capital. The palace and Noble museum are but a couple of the great buildings in the old town. By boat you can really appreciate the uniqueness of the city as it spreads out across many islands all interconnected in some way. It certainly is one of the most interesting & beautiful cities in the world and has the must visit ABBA collection!!
The old city is a magical labyrinth of cobblestone and majestic buildings - rising higher than I thought would be the case. Each seeking out the light and colored in different facade hues. Of course any city centre is filled with tourist shops, but for some reason Stockholm’s heart doesn't seem overly commercial. Above all it’s the ambience of sophisticated posture and calm that permeates the capital. The palace and Noble museum are but a couple of the great buildings in the old town. By boat you can really appreciate the uniqueness of the city as it spreads out across many islands all interconnected in some way. It certainly is one of the most interesting & beautiful cities in the world and has the must visit ABBA collection!!Onto the science. Well a little rain and traffic to get there but well worth it as Karolinska Institute is well known for its prowess and was hosting a seminar on the Aging Brain in association with EuroStemCell and the ISSCR. I was a little late due to the weather so I arrived just as the talks were starting and settled in to listen.
Four great speakers made presentation, moderated by Professor Arenas Ernest of Karolinska.
What stuck me as interesting was that the brain evidentially has pockets of stem cells which aren’t known to be regenerative but may have the potential, if activated, to proliferate. Magdaline Gotz was adamant that her focus on Radial Glial Cells would prove beneficial as a potential personalised restorative pathway of new brain tissue. Her work on the topic can be found at her link below and also via youtube here and is is very exciting.
What stuck me as interesting was that the brain evidentially has pockets of stem cells which aren’t known to be regenerative but may have the potential, if activated, to proliferate. Magdaline Gotz was adamant that her focus on Radial Glial Cells would prove beneficial as a potential personalised restorative pathway of new brain tissue. Her work on the topic can be found at her link below and also via youtube here and is is very exciting.
 |
| Magdalena Gotz, PhD - Malin Parmar, PhD - Per Svenningsson, MD, PhD - Fred “Rusty” Gage, PhD |
As a patient focused translational analyst I look out for those programs that have nearish term impact value. In this case Malin Parmar of the Lund University in Sweden has a long history battling Parkinson’s disease and noted the pioneering fetal work done in the past and restarted recently under the TransEuro initiative to trial fetal derived dopamine producing neurons. This approach was shown to be effective in certain patients yet had a 25% risk factor on adverse events. With the new protocol they hope to improve on that inefficiency with a pan-European effort to study the approach again. In the meantime Malin and her collaborators are in pre-clinical development on hESC derived dopaminergic neurons with a timeline to being in the clinic by 2018. I have previously featured her work in the Pluripotent section of the blog here (a few sections in).
To close out the presentations Fred (“Rusty”) Gage of the Salk Institute made a wonderfully positive talk on the ability of the human brain to be proliferative if stimulated by activity and learning. Studies were shown to prove the point and indeed it’s this authors firm belief that the more you remain active and curious throughout your life the more you can improve your cognitive ability even in a disease state. So the take home was stimulate those brain cells by being sporty and curious into your late years and you’ll battle on healthier and more able.
Post meeting I got a chance to chat with Malin briefly about the state of play with the planned pluripotent ISC-hpNSC Parkinson trial and embryonic derivation issues in Europe. She wasn’t sure of the parthenogenetic cell line approval in Europe at this stage and that Karolinska had developed a proprietary hESC line using xeno-free conditions (more on that in another post). I noted some of the legal issues and commented on the inaccessibility factor in current procedural approaches to treatments for cell transplantation into the brain. Gen 2 & 3 therapies may be more universal given the potential for systemic or non-surgical applications.
GL of course to all those in this area as it’s a major challenge which has so many unmet medical conditions.
Next up in a couple of days will be some coverage at convention centre.
Cheers
________________________________________________________________
Cheers
________________________________________________________________
One of the great aspects of attending science shows is the knowledge base assembled to impart data and findings... on occasion wisdom and advice. The latter was the case for the 1st Focus Session I attended off and on during Wednesday morning. The speakers were all seasoned and came across as genuine in their effort to impart guidance on a less than formulaic bench to bedside roadmap. A few of the names on the podium, while I was there, made a number of good points and a couple which I noted down as iffy...
Use lawyers that have a contingency based dev account - not such a bad idea if they’re game. I know from battling a News Corp. division that it works if you can get your legal team to buy-in… (we won btw so they were happy to recoup & profit). Not sure how practical that is for a young researcher without a track-record...
Road-test your pitch to VCs without any intention to take their money - again sounds good, if not a bit Machiavellian… the more you practice & hone the story the better definitely... who knows you may even get lucky and one of the least likely “trialist” money men will spring for it
Be prepared for rejection - that’s sound advice! It takes stamina to succeed and know how to turn rejection into enhancement and energy - stay the course is a good mantra
Don't inhibit tech transfer to squeeze the deal making - this is one of those iffy ones, sounded a bit too much like a justification for commercial realities that are lop sided
Money will find good ideas - somewhat true but mostly money follows money and track records
Management are commodities - hired hands indeed run a tight ship and get rewarded for being efficient and clinical in their methodology, that’s positive on the one hand but I would say it depends entirely on the type of culture and organisation it is - there are situations which require a vested innovative leader that was born with the passion for the venture & drives it...
Some of the speakers while I attended where:
Ken Chien Group of Karolinska
Robert Millman - Semma Therapeutics - see also PaulK's Blog post
After the presentations I had a moment with Hans Keirstead regarding his eye work, which he relayed was very much on with 3 dedicated scientists to the project and that they were focused on developing a RPE/Photoreceptor transplant using 3D culture technology. We weren't able to finishing the conversation as time was short and his departure from the event early made a request for a follow-up sit down not possible.
All the Focus Sessions were 3 hours, so I took the opportunity to move between a few during the morning.
I stopped in for Jeanne Loring, of The Scripps Research Institute, presentation in the Stem Cell Engineering Session...
I’ve always try to catch what Jeanne says, as I respect her opinion and like her frank style. This bore out in my interview with her later during the show, which I will do a separate piece on. Jeanne presented a 2 year study of stem cell engineering sponsored by the NSF, NCI, NIH and the NIST (abstract & quote "from this assessment, the panel concluded that there needs to be an increased role for engineers and the engineering approach.."
A few things stood out - the solid two year research done primarily by Robert Nerem, PhD, was a monumental task and an example of endurance that is routinely taken on by scientists...
On the hESC front it seems manual passage using MEF is the most stable long term for hESC versus alternatives which showed passage deletions in gene52 but not in MEF cultures.
Also Jeanne said that the FDA is not bothered with MEF culture use and it’s not an inhibitor to translation.
One further bit I had noted was that Japan is requiring whole genome sequencing - we can see that is important given the recent iPS RPE issue with a detected gene mutation in the final validation step.
 One of the other session halls was featuring Stem Cell Banking and I stopped in to see what was being discussed. The advent of banking of pluripotent stem cell lines - notably the iPS initiatives - were well covered and the resource and QA aspects outlined. Given the history of the hESC initiatives and requirements for regulatory documentation the basic frameworks were existing but updated and adapted to include iPS now. Two good ports of call for more information are the hPSCreg and EBiSC resources.
One of the other session halls was featuring Stem Cell Banking and I stopped in to see what was being discussed. The advent of banking of pluripotent stem cell lines - notably the iPS initiatives - were well covered and the resource and QA aspects outlined. Given the history of the hESC initiatives and requirements for regulatory documentation the basic frameworks were existing but updated and adapted to include iPS now. Two good ports of call for more information are the hPSCreg and EBiSC resources.
Last up for this post is the exhibitor review I had with Luke Dimasi, a Product Manager at Corning Life Sciences. I was interested in their new product distribution arrangement with BioLamina for their rLaminin-521 which Corning is launching under the trade name “PureCoat.”
To make a long story short BioLamina are an innovative Swedish biotech company affiliated with Karolinska Institute pioneering recombinant laminin products as cultureware. Their xeno-free, chemically defined and feeder-free system has been integrated by Corning into a robust line of PureCoat surface flasks for the lab.
I have followed this technology as it has been published and is a patent pending innovation as a solution for Pluripotent cell differentiation. It is noted as an highly efficient method to expand cells in a scalable cGMP manner. Also a 3D micro-carrier Gen 2 product awaits in the pipe...
To close this type of service sector development, along with the productization of similar biomaterials, such as those out of the Langer Lab, are enabling technologies for success.
More to follow...
Cheers
_____________________________________________________________________
________________________________________________________________
 MT: Yes, a little background. I started in 2000 with ES cells and proved in mid-2000 using primate ES cells that we could treat some retinal diseases but we hesitated to move to the clinical stage because the risk of immune rejection. By that time iPS cells came out and I was very happy as I knew the last hurdle would be solved w/ iPS cells so we immediately started research using those cells and after 5 to 6 years of translational research in preclinical studies we started the 1st patient clinical application last September and we will judge the safety and effect 1 year later this September. We announced mid-term results in March and so far we don’t observe any immune rejection without any immunosuppression, which we expected as a result of using autologous iPS cells.
MT: Yes, a little background. I started in 2000 with ES cells and proved in mid-2000 using primate ES cells that we could treat some retinal diseases but we hesitated to move to the clinical stage because the risk of immune rejection. By that time iPS cells came out and I was very happy as I knew the last hurdle would be solved w/ iPS cells so we immediately started research using those cells and after 5 to 6 years of translational research in preclinical studies we started the 1st patient clinical application last September and we will judge the safety and effect 1 year later this September. We announced mid-term results in March and so far we don’t observe any immune rejection without any immunosuppression, which we expected as a result of using autologous iPS cells.
 MT: In the near future. We made a start-up company, Healios, they made an IPO last week, they plan to do a clinical trial in 2 or 3 years time in the US as they need the time to apply the protocol. [see also Riken tab in this blog]
MT: In the near future. We made a start-up company, Healios, they made an IPO last week, they plan to do a clinical trial in 2 or 3 years time in the US as they need the time to apply the protocol. [see also Riken tab in this blog]
 MT: The people who don’t know the disease think the big sheet is the best but there are many, various situations with the disease, various stages, various lesion sizes, so some patients need a large sheet. Ours is 1 x 3mm, people in the US are preparing a 3 x 5mm sheet, so some people don’t need such a big sheet and earlier stage patients don’t require a big incision, so cell suspension is more feasible.
MT: The people who don’t know the disease think the big sheet is the best but there are many, various situations with the disease, various stages, various lesion sizes, so some patients need a large sheet. Ours is 1 x 3mm, people in the US are preparing a 3 x 5mm sheet, so some people don’t need such a big sheet and earlier stage patients don’t require a big incision, so cell suspension is more feasible.
 MT: MSCs are safe. iPS/ES are hard to control so are limited to institutes that can maintain them/control them properly but the industrialization for a standard treatment iPS/ES is very good because we can have one lot otherwise many donors and always a lot of changes so that’s not very good industrially. In the future the ES & iPS cells people can control will be the way to industrialize and standardize treatment.
MT: MSCs are safe. iPS/ES are hard to control so are limited to institutes that can maintain them/control them properly but the industrialization for a standard treatment iPS/ES is very good because we can have one lot otherwise many donors and always a lot of changes so that’s not very good industrially. In the future the ES & iPS cells people can control will be the way to industrialize and standardize treatment.
 MT: For the company it’s an issue - I don’t care. Patients don’t care. Healios is very good and they are in contact with the NIH group and the Ali group (UCL) - maybe they collect good procedures from the world.
MT: For the company it’s an issue - I don’t care. Patients don’t care. Healios is very good and they are in contact with the NIH group and the Ali group (UCL) - maybe they collect good procedures from the world.
 Who wouldn't want to believe in a solution for age related degenerative conditions via a shot, transplant or cell stimulant. It’s the ultimate product - one, if produced, would mint the next superpower in the guise of an all powerful corporate entity. Hopefully with a humanitarian bent for universal application and charity - otherwise we're in for the equivalent of eugenics, not via genetic engineering but through class access.
Who wouldn't want to believe in a solution for age related degenerative conditions via a shot, transplant or cell stimulant. It’s the ultimate product - one, if produced, would mint the next superpower in the guise of an all powerful corporate entity. Hopefully with a humanitarian bent for universal application and charity - otherwise we're in for the equivalent of eugenics, not via genetic engineering but through class access.
 Amy Wagers of Harvard, who leads the team that presented the controversial data on GDF11, again presented data during the closing Plenary session at ISSCR 2015. She reiterated that GDF11 was indeed responsible for stimulating the rejuvenation of aged tissue. What was interesting was her resounding affirmation of her previous team’s work with additional clarification of the decrease in aged sampling while postulated the reasons for metabolic interaction. With this new evidence it seems there is a case for continued debate between Novartis and Wager’s group - with the ball now firmly in the big pharma’s court.
Amy Wagers of Harvard, who leads the team that presented the controversial data on GDF11, again presented data during the closing Plenary session at ISSCR 2015. She reiterated that GDF11 was indeed responsible for stimulating the rejuvenation of aged tissue. What was interesting was her resounding affirmation of her previous team’s work with additional clarification of the decrease in aged sampling while postulated the reasons for metabolic interaction. With this new evidence it seems there is a case for continued debate between Novartis and Wager’s group - with the ball now firmly in the big pharma’s court.
The last of the three sessions I will relay here is the talk by Mitsutoshi Yamada, a postdoc fellow who works with Dieter Elgi’s at the New York Stem Cell Foundation (“NYSCF”). What I took away from the talk was the viability issue of using screening technology to assist in the process of ensuring safe and effective translation of mitochondrial replacement therapy. It was shown in this study that there was no adverse developmental effects using the NT process, which seemed positive and that there was also solid reporting of integrity analysis. The issue of reported “drift” I believe was tweeted once or twice on the presentation at the time, which was a noted issue requiring follow-up. Paper to be published shortly.
As mitochondrial replacement therapy is being considered in the US and the legal authorization to proceed in the UK allowed it’s fitting that the science investigation continues apace to answer the open questions and look to increase the accumulating knowledge surrounding the technology. Infertility is a curse and a growing problem in today’s stress filled and environmentally polluted world.
 This sculpture by my Mother was created some ten years ago for all those women that suffer from infertility - she’s screaming to the heavens…it weighs 500 kilos and was made in Norway of granite - it rests now in the Pyrenees, closer to the sky...
This sculpture by my Mother was created some ten years ago for all those women that suffer from infertility - she’s screaming to the heavens…it weighs 500 kilos and was made in Norway of granite - it rests now in the Pyrenees, closer to the sky...
____________________________________________________
 Prof. Austin Smith stated focus is in trying to “understand the relationship between stem cells in culture and cells in the embryo, which are not stem cells because they don’t self-renew. So we’re trying to understand how cells that we can grow in the culture dish relate to real developmental entities in the embryo of mice or, of course, ultimately of humans.”
Prof. Austin Smith stated focus is in trying to “understand the relationship between stem cells in culture and cells in the embryo, which are not stem cells because they don’t self-renew. So we’re trying to understand how cells that we can grow in the culture dish relate to real developmental entities in the embryo of mice or, of course, ultimately of humans.”
 Jeanne Loring’s view of this is somewhat more pragmatic, having also based her early career in the science on the study of mouse ES cells: “I decided to learn one thing and then move on and learn another and then try to put them together…. I have the mouse ES history, which I share with Austin and Rudolf… human cells don’t act like mouse cells, they’re much harder to grow... whether you can make a human cell with the quality of a mouse” is still being investigated “I just went straight to human pluripotent stem cells and realized they were not going to be like mouse and lived with it… so I just bypassed that… my cells become what I want them to become and that’s it - I’m done.. they don’t need to be mouse cells, they’re human cells”
Jeanne Loring’s view of this is somewhat more pragmatic, having also based her early career in the science on the study of mouse ES cells: “I decided to learn one thing and then move on and learn another and then try to put them together…. I have the mouse ES history, which I share with Austin and Rudolf… human cells don’t act like mouse cells, they’re much harder to grow... whether you can make a human cell with the quality of a mouse” is still being investigated “I just went straight to human pluripotent stem cells and realized they were not going to be like mouse and lived with it… so I just bypassed that… my cells become what I want them to become and that’s it - I’m done.. they don’t need to be mouse cells, they’re human cells”

 Jeanne Loring of the Scripps Research Institute in La Jolla California kindly sat down with me at the ISSCR annual meeting for a broad discussion of her history, views on the field and developments in the science.
Jeanne Loring of the Scripps Research Institute in La Jolla California kindly sat down with me at the ISSCR annual meeting for a broad discussion of her history, views on the field and developments in the science.
 JL: So I was trained in embryology and neurobiology, I studied neural crest cells which are actually stem cells and I was fascinated by them. Then when I finished graduate school I got a job as an assistant professor at the University of California Davis and I then realized I could either teach or do research but not both. There were not enough hours in the day, so I took the opportunity to join a biotech company in California called Hana Biologics. There were lots of them around, in 1987. I joined specifically because they were planning a stem cell therapy for Parkinson’s disease. I thought I could use what I thought was practical because I was getting a little bit tired of generating just knowledge. I wanted to generate practical knowledge which made me a little bit different from everybody else at the time.
JL: So I was trained in embryology and neurobiology, I studied neural crest cells which are actually stem cells and I was fascinated by them. Then when I finished graduate school I got a job as an assistant professor at the University of California Davis and I then realized I could either teach or do research but not both. There were not enough hours in the day, so I took the opportunity to join a biotech company in California called Hana Biologics. There were lots of them around, in 1987. I joined specifically because they were planning a stem cell therapy for Parkinson’s disease. I thought I could use what I thought was practical because I was getting a little bit tired of generating just knowledge. I wanted to generate practical knowledge which made me a little bit different from everybody else at the time.
M: Your independent in an academic setting now.
 JL: Well they’ve done that too. Yeah, the essence of our approach with endangered animals is to take the pluripotent stem cells and to use the technologies that has been developed for mouse and for humans and make gametes out of the cells. Then use IVF technology, that is also in development for these animals, and have a surrogate host that we’ll be able to put the embryos into and regenerate the species. Just a small thing! I’m doing it with the Northern White Rhino, as there are only 5 of them left. There’s only one male and the females I think, with one exception, are beyond reproductive age and they’re dying.
JL: Well they’ve done that too. Yeah, the essence of our approach with endangered animals is to take the pluripotent stem cells and to use the technologies that has been developed for mouse and for humans and make gametes out of the cells. Then use IVF technology, that is also in development for these animals, and have a surrogate host that we’ll be able to put the embryos into and regenerate the species. Just a small thing! I’m doing it with the Northern White Rhino, as there are only 5 of them left. There’s only one male and the females I think, with one exception, are beyond reproductive age and they’re dying.
M: Which zoo is that?
_____________________________________________________________________
Media Hype | ESi Bio | CIRM's Chairman
Along with the full schedule of simultaneous science sessions, showcases, exhibitors and posters - there were a couple of dedicated media presentations which were part of the organizers’ outreach effort. One such presentation was directed at delving into the social and ethics issues surrounding experimental stem cell treatments. Always a topical issue, more so now perhaps as the sector is growing and initial advances are being reported. There is still a long way to go before a full range of approved therapeutics are available and as such it’s a challenge to ensure the public is informed accurately. As a dedicated society for the sector the ISSCR is a leading voice and active participate in the collaborative management of an internationally complex set of issues to ensure safe and beneficial treatments are correctly positioned to the public.
This challenge is not solely the domain of a few industry organisations but, as the media presentation panel members suggest, is the multi-faceted community at large’s responsibility to build the bridges between the science and the patients seeking solutions.
The title of the event Promise, Progress and Hype reflected the content of the presentations by the speakers who were “representatives involved at home and internationally in ethical, social and patient care issues associated with stem cell science and experimental treatments.”
 |
| Jeremy | Tim | Ira | Dan | Megan |
Moderator: Jeremy Sugarman, M.D., M.P.H., M.A., John Hopkins Berman Institute of Bioethics,
Panelists: Timothy Caulfield, LL.M., Health Law Science Policy Group, University of Alberta, Ira Herrmann, Stem Cell Network NRW, Düsseldorf, Dan Kaufman, M.D., Ph.D., University of Minnesota, Megan Munsie, Ph.D., Stem Cells Australia.
A featured aspect of the talk was the new “Closer Look at Stem Cells” website, which is “an online resource to help patients and their families make informed decisions about stem cell treatments, clinics and their health.” This portal will look to serve as a gateway to the public and hopefully bridge the gap that exists from a patient’s perspective in fully understanding the potential and what is currently being developed, in the clinic, and to inform as to the pitfalls of the commercial treatments being offered in unregulated environments. A comprehensive ISSCR Patient Handbook is available via their website.
A few quotes from the media literature on the topic:
“I am often contacted by patients struggling with very difficult decisions about their health, and who want to know more about the potential of stem cells,” said Larry Goldstein, a stem cell scientist at the University of California, San Diego and a member of the ISSCR task force responsible for the website expansion. “My experience is that understanding the current state of stem cell science and medicine is key to making informed decisions about stem cell treatments, and so I encourage patients to start their journey on the ‘Closer Look at Stem Cells’ website.”
“The ‘Closer Look at Stem Cells’ website is a direct channel from researchers to the public,” said Megan Munsie, a scientist with Stem Cells Australia and chairperson of the ISSCR task force responsible for the website expansion. “Promising clinical trials are underway for many diseases and conditions, but most stem cell-based treatments are still in the future. We hope that the website will foster interest and excitement in the science, but also an understanding of the current limitations of stem cells as medicine and a healthy skepticism of clinics selling treatments.”
On a number of fronts the community is making a serious effort to tackle the issues head-on and make forward progress in meeting the public’s request for information and feedback. There is nothing worse that being in a desperate situation without knowledge nor recourse so from my perspective it’s a fundamentally important part of the puzzle that requires outreach and more outreach. I’m encouraged to see such great work being done on this topic from the centre…
My observational notes -
One point I had was related to the subjective nature of informed consent in varied jurisdictions and the perception of model systems being applicable to the whole when nature is a diverse set of realities - economic, societal, ethical and legal are few that define the difference…
Also, patient criteria for treatment success varies widely - even in the west. Beyond informed consent there is the reality of moderate to ineffective solutions being sold on the basis of overreach in a commercial setting, which can equally be applicable to many industries. Right to Try is a grassroots call for solutions - can that momentum can be a driver for positive restructuring is the op. How expansive will any net be in curtailing safe product approvals with less that optimal results that don't meet expectations due to exploitive sales tactics? Can and should the industry itself push to establish minimum stem cell treatment criterias for efficacy before products are approved by regulators? What about those countries that don't follow the internationally agreed guidelines? Lot’s of Qs here…
Onto an exhibitor which caught my attention, ESi Bio, a division of BioTime. I was curious to understand more about their positioning and science, beyond their being a leading hESC source & derivative progenitor cell line service provider and some of the historical industry interconnections.
First off I got the division mixed up with the Singapore subsidiary ES Cell Int. (“ESI”), under the same corporate umbrella. ESI Bio in San Diego is the management & technical team working alongside BioTime corporate and arm’s length from ES Cell International in Singapore, an acquired subsidiary of BioTime. However, the ESI Singapore products are the interconnect as the San Diego team are marketing their cell line. Recent deals with the UK, Inserm in France and City of Hope/CIRM in CA were all driven by this San Diego team. I met with Stephanie & James plus a couple of the group’s support scientists & a marketing exec.
A few take-aways from the chats I had with the team and the more detailed biz review meeting I had with Stephanie & James -
- Biotime is a diverse and interwoven company with many moving parts
- hESC lines & progenitors are known and entering the market now with 3rd party program deals starting to be publically announced. This is an indication of the growing interest in hESC translational sci.
- iPS developer kits using mRNA are being positioned as a product rather than a service
- BioLamina and BioTime/ESi have a link, in what shape or form wasn’t expanded on
- BioTime considers it a good faith gesture to have a License to Japan Academia’s iPS tech for mRNA derivation even though there is an acknowledged freedom to operate scope in the sector. Michael West et al’s history with OCT4 in early reprogramming work was noted.
- The overall umbrella of BioTime & its technology base is leading edge - from it’s Hydrogel tech, to it’s Pluripotent cell derivation technology, LifeMap et al to its proprietary therapeutics and diagnostic subs..
To finish up this post I wanted to relay some thoughts on the meeting I had with one of the Industry’s leaders, Mr. Jonathan Thomas, Chairman of CIRM.
Prior to ISSCR2015 I had sent a short note to Kevin McCormack to ask who was attending, as I wished to introduce myself. Kevin relayed, in his engaging manner, than he couldn’t find an excuse to justify making it over but that Mr. Thomas and Dr. Mills were attending and would no doubt be happy to meet up. Unfortunately Dr. Mills couldn’t attend the event so I arranged to talk with Mr. Thomas.
Of course being interested in Swedish culture we coincidentally found ourselves in the same mode at the same time prior to the show - touring the old city. The difference being I was solo and Jon was touring with an entourage and had a guide pointing things out - very cool! I of course recognised the stature and mustache from afar, while having a juice and muffin at a cafe on the central square.
Next was the opening plenary sessions which were held in the main forum which holds 3000+, a great space which was packed for a number of sessions during the event. I like to sit on the aisle at these presentations, nearish to rear, so I can move when necessary without disturbing anyone. Well here we go again, Jon turns up and does the same thing - sits on the aisle on the other side! Funny I thought.
Next day I meet a classic American gentleman - one which I can only describe as resembling a favorite actor of mine, Sam Elliot, and a dear family friend of my Mother’s whom I'll be visiting in Normandy next month (same moustache and stature - minus the grey!).
Given Jon was evidently busy I didn’t wish to delay him too much and introduced myself and relayed a few strategic thoughts, as per the CIRM’s outreach request, and offered my assistance in any way to further the good cause.
My strategic plan thoughts related to -
- Method of Action research shouldn’t delay translational benefits to patients if safe
- More International collaborations
- Need for new financing model for the industry. Existing reliance on Pharma model not proving to be effective for SC industry. De-Risking via territorial pre-sales suggested and control destiny more w/ marketing/distribution partnerships with Pharma (win/win).
- Public engagement needs to be a priority, alongside Advocacy group participation. Direct contact and awareness factor - translating & bridging science.
- Alpha Clinics as a managed route to market can be expanded through out-of-state activities, franchising and a branded accreditation program. Control destiny again.
- First Look schemes for Pharma/Bio for tie-in & info-flow.
- IP participation/partnerships, ROI.
I’m sure most if not all of these discussions points have been considered, especially the finance modelling, given leadership’s background. I was pleased to see a Town Hall announcement for the excellent CIRM HIV programs on the public awareness front. I trust inflection will happen but good to have plan B & C….
Well that does it for now - I’ll be writing more next week and wish everyone in the US a happy Independence Day holiday weekend. Here I’m off the the mountains, as it’s stiflingly hot and humid at the moment, to cook some burgers for the family (must remember the Heinz!).
Cheers ________________________________________________________________
Masayo Takahashi - "Hope - Yes" & "Patients First"
Having followed closely the developments in programs using pluripotent based therapeutics I was fortunate during ISSCR2015 to have the opportunity to sit down with Dr Masayo Takahashi to discuss her pioneering efforts to translate Shinya Yamanaka’s groundbreaking iPS technology for debilitating retinal conditions.
As most everyone is aware, the first iteration of the program, for advanced Wet AMD, has entered the clinic and been safely administered to the first patient - a milestone achievement for the field, which has been widely covered by the media, especially in Japan. However, as I learned first hand, this first step is but a part of a comprehensive strategy to address most retinal diseases by way of various cultured cell transplantation methods, depending on the patient condition - including suspension therapies and multi-layered organoid developed tissue. This was best described by Masayo “what I have said to the Japanese regulators is that ideally we need all cell types - sheets, suspensions, auto, allo - and the surgeons will choose which to use for each patient.”
Before relaying the key segments of the interview, I wanted to express some thoughts of how practical and committed to the patient Masayo is. Her clinical practice is at the very heart of her professional vision - to bring relief to those that come to her for help. Disappointment again and again in not being able to help drives her passion for new therapies. She is both confident and open to the process that has already taken more than a decade and a half of her research. The goal being, in time, to have all the tools necessary to deliver on the promise to her patients and fulfill on that hope, that is very real and apparent today - something she couldn’t point to just a few short years ago. Her new message is very clear now “visual impairment is not as bad as they think and you can change that world - so there is hope - yes.”
Cheers
Interview:
Q: There is a lot of hype in the field how have you addressed that?
MT: When I started to do the regenerative medicine work the media broadcast our efforts and many patients came and they expected I could help them. But 10 years ago I was very nervous because after hearing the news they were disappointed in front of me so I started to talk to the media and educate. Every month we worked with media so gradually within this period they learned and suppressed their expectations so in Japan the hype isn’t so high anymore.
Q: Does the internet makes things easier for patients to understand?
MT: People who can connect with the internet can understand but the older people still don’t have access to the internet and rely on the newspaper and TV but sometimes they’re informed wrongly as a result so I still struggle.
Q: Is that due to the technical language and complexity of the science?
MT: Common sense is different from the medical reality but the regenerative medicine area is very focused so we can use the media to inform the public correctly. Regenerative medicine won’t cure everything but if you think in a different way you can do many things. The “hope” should be the correct one. People need to learn the way of thinking of the scientists - in Japan people are very clever and gradually they have understood. So if you teach correctly they can understand gradually. Its important to relay the correct information. Media sometimes tries to simplify as a need or belief in the communication method yet they loose the true message. Stem cells are a specific area with many unknowns - yes - it’s like a “black box.”
Q: You started using ES neuronal cells then moved to iPS and retinal cells
 MT: Yes, a little background. I started in 2000 with ES cells and proved in mid-2000 using primate ES cells that we could treat some retinal diseases but we hesitated to move to the clinical stage because the risk of immune rejection. By that time iPS cells came out and I was very happy as I knew the last hurdle would be solved w/ iPS cells so we immediately started research using those cells and after 5 to 6 years of translational research in preclinical studies we started the 1st patient clinical application last September and we will judge the safety and effect 1 year later this September. We announced mid-term results in March and so far we don’t observe any immune rejection without any immunosuppression, which we expected as a result of using autologous iPS cells.
MT: Yes, a little background. I started in 2000 with ES cells and proved in mid-2000 using primate ES cells that we could treat some retinal diseases but we hesitated to move to the clinical stage because the risk of immune rejection. By that time iPS cells came out and I was very happy as I knew the last hurdle would be solved w/ iPS cells so we immediately started research using those cells and after 5 to 6 years of translational research in preclinical studies we started the 1st patient clinical application last September and we will judge the safety and effect 1 year later this September. We announced mid-term results in March and so far we don’t observe any immune rejection without any immunosuppression, which we expected as a result of using autologous iPS cells.
There was a famous paper in the journal Nature that the autologous iPS cell invoked immune rejection in a mouse model but I think the research design wasn’t very good. They transplanted kind of a tumor which would be rejected - not the iPS cells but the tumor.
Q: Was the surgery difficult for the lady (1st patient)
MT: Yes the surgery was the most risky part. We were worried a little but the procedure was successful with no adverse events so far.
Q: And the next patient?
MT: We tried, we prepared but decided to go quickly to the allogeneic because the cells are already there from Shinya Yamanaka’s cell line stock. He made the 1st iPS cell line and they have come to our lab.
Q: Have they been approved as clinical grade by the Japanese regulators?
MT: Yes but about the protocol, we will apply within this year for approval. We should reapply as it’s allogeneic, different from autologous.
Q: Will this line be available to others?
MT: Shinya Yamanaka will distribute to various centers with one of the institutions being mine. So there will be a Spinal Cord Injury protocol, maybe the Parkinson’s disease trial will go to an allogeneic protocol, the hematopoietic (platelets) will also. So the various protocols will use that cell stock.
Q: Japan is moving very quickly, is that of concern in the community or is that in your mind appropriate?
MT: Most patients are supportive but some people worry we move too fast but really we prepared, labored and accumulated the data and the people who don’t know the whole data usually say you have the risk - that’s very stressful. So actually we don’t care what they say because they don’t know. Maybe it’s a social balance.
Q: Are you taking the trials overseas, outside of your home market?
 MT: In the near future. We made a start-up company, Healios, they made an IPO last week, they plan to do a clinical trial in 2 or 3 years time in the US as they need the time to apply the protocol. [see also Riken tab in this blog]
MT: In the near future. We made a start-up company, Healios, they made an IPO last week, they plan to do a clinical trial in 2 or 3 years time in the US as they need the time to apply the protocol. [see also Riken tab in this blog]
Q: I’d like to get your opinion on the use of a monolayer versus the selection of a suspension protocol.
 MT: The people who don’t know the disease think the big sheet is the best but there are many, various situations with the disease, various stages, various lesion sizes, so some patients need a large sheet. Ours is 1 x 3mm, people in the US are preparing a 3 x 5mm sheet, so some people don’t need such a big sheet and earlier stage patients don’t require a big incision, so cell suspension is more feasible.
MT: The people who don’t know the disease think the big sheet is the best but there are many, various situations with the disease, various stages, various lesion sizes, so some patients need a large sheet. Ours is 1 x 3mm, people in the US are preparing a 3 x 5mm sheet, so some people don’t need such a big sheet and earlier stage patients don’t require a big incision, so cell suspension is more feasible.
Q: What is your current disease state target?
MT: Advanced Wet AMD and we pull out the neovascular tissue, so a big defect of RPE, and cell sheets are appropriate but if the neovascular damage isn’t large we don’t want to cut and therefore cell suspension is better.
Q: The market is fragmented - is there a synergy with other programs?
MT: The regenerative medicine area is different than the small molecules, it’s more adaptable, so the judgement should return to the clinical scene and not the big pharma. The clinical reality will determine application and the Japanese government knows very well about this issue and we cooperated to make the new law. The Ministry of Health accepted that regenerative medicine is different than small molecules and that all is needed is a small number of patients to get approval, which is a great advance, a revolution.
Q: Is safety sufficient in a small population study?
MT: Of course the accumulation of the animal data needs to be reconfirmed by 10 or so patients for safety but the statistical significance of the efficacy needs more patients to prove the probable efficacy. Companies can sell the products based on smaller numbers so we don’t need big big pharma for promoting regenerative medicine. Companies can sell but they must register and prove efficacy within 7 years with regular exams. Success will be a collaboration between regulatory and academia with insurance reimbursement playing a commercial role which is incredible and kind of a risky law. The background of that is that academia promoted the regenerative medicine mainly so we cooperate very tightly with government and will decide where to provide treatment after approval with rules later.
Q: Do you plan enhanced cell products?
MT: Manipulated cells can work better, yes. So far natural cells are the most feasible, as regulators don’t like manipulated cells or “supercells.” In future but for now natural cells are good.
Q: Can you speak to the adult cell types
 MT: MSCs are safe. iPS/ES are hard to control so are limited to institutes that can maintain them/control them properly but the industrialization for a standard treatment iPS/ES is very good because we can have one lot otherwise many donors and always a lot of changes so that’s not very good industrially. In the future the ES & iPS cells people can control will be the way to industrialize and standardize treatment.
MT: MSCs are safe. iPS/ES are hard to control so are limited to institutes that can maintain them/control them properly but the industrialization for a standard treatment iPS/ES is very good because we can have one lot otherwise many donors and always a lot of changes so that’s not very good industrially. In the future the ES & iPS cells people can control will be the way to industrialize and standardize treatment.
Q: What are your future plans / next steps:
MT: Our next steps are to have combined stem cell sheets - not only RPE but RPE with Photoreceptors and perhaps the vessel layer. Like a dream in our institute, that has a very high developmental biology focus, we talk about the whole retina with blood vessels and will try to deliver the entire retina for retinal disease conditions that destroy all the layers. For now we are working on monolayers, suspension, photoreceptors, combined layers and ganglion etc with 2016 for the allo, 2017 for the Healios suspension and 2018 for the photoreceptors.
MT: We are not actually collaborating. We have a communication and information exchange, like a think tank. We know how they promote and we are doing very well. We don’t have to hide. They use similar technology adapted from our work. The aim is to make a standard treatment.
Q: Is ownership not an issue?
 MT: For the company it’s an issue - I don’t care. Patients don’t care. Healios is very good and they are in contact with the NIH group and the Ali group (UCL) - maybe they collect good procedures from the world.
MT: For the company it’s an issue - I don’t care. Patients don’t care. Healios is very good and they are in contact with the NIH group and the Ali group (UCL) - maybe they collect good procedures from the world.
Q: Are companies in Japan looking at this sector as a team approach - does this help?
MT: Yes, society of regenerative medicine companies in Japan are maybe 100 companies now under the F.I.R.M association. Fuji, industry, pharma - all diverse companies. Not as a Keiretsu but more an association. Companies are now interested unlike 5 or 6 years ago. I told many companies to help us but they didn’t in the beginning but now they do. The government has helped a lot having supported the industry 10 years ago but they see the reality now as we have the clinical application.
Q: How do you see yourself, as a leader, role model - is there pressure?
MT: Shinya Yamanaka is like an Emperor now - everyone adores him. About the pressure, we have accumulated the data so I don’t fear anything. I have a scheme for 10 years plus and a plan. I know all - from the cells, the pluripotency, genes, animals, disease, patients and social and no worries only a process to move along. There are some against us but if I listen to their talks I’m not convinced by them, I mean persuaded, something wrong in their logic. As a role model - maybe I should behave myself! Patients happiness is what I believe - not papers or money, not interested. Patients first, outpatient clinic is very important to me.
Q: How do you view Lucentis/Eylea?
MT: Wonderful - we saw AMD 25 years ago and there was nothing at all. So we just explained the disease as incurable for 10 years but finally it came out, it was wonderful. We knew AMD very well and knew Lucentis wouldn’t cure everything. The treated patient had 10 injections before surgery and her condition deteriorated from 0.3 to less than 0.1 even though she had the available treatment, so we stabilized her visual acuity with radical treatment without any injection.
_____________________________________________________
GDF11 | Adult MSCs > MS | NYSCF Mito/NT
While I attended many sessions during the week at ISSCR 2015, a few caught my attention. Those were topical for me as they touched on some previous
reporting I had done and featured updated information which I want to share.
As a non-scientist the finer details of the technical presentations I leave to the experts. However, as I appreciated from Rusty Gage's talk pushing those neurons to bridge helps... I try to do my homework and as an objective observer I process that in relation to how it might impact the field and patients in particular.
So in that spirit onto the highlights - GDF11 first.
The fountain of youth, as it was often referred to when young blood was first presented as the ultimate elixir. The property identified within the crimson tide was GDF11, a protein that evidentially is in abundance in young blood but over time depletes to the point where its reduced percentage in aged blood has been identified as the potential treatment target for restorative therapeutics. Enter the debate...
So in that spirit onto the highlights - GDF11 first.
The fountain of youth, as it was often referred to when young blood was first presented as the ultimate elixir. The property identified within the crimson tide was GDF11, a protein that evidentially is in abundance in young blood but over time depletes to the point where its reduced percentage in aged blood has been identified as the potential treatment target for restorative therapeutics. Enter the debate...
 Who wouldn't want to believe in a solution for age related degenerative conditions via a shot, transplant or cell stimulant. It’s the ultimate product - one, if produced, would mint the next superpower in the guise of an all powerful corporate entity. Hopefully with a humanitarian bent for universal application and charity - otherwise we're in for the equivalent of eugenics, not via genetic engineering but through class access.
Who wouldn't want to believe in a solution for age related degenerative conditions via a shot, transplant or cell stimulant. It’s the ultimate product - one, if produced, would mint the next superpower in the guise of an all powerful corporate entity. Hopefully with a humanitarian bent for universal application and charity - otherwise we're in for the equivalent of eugenics, not via genetic engineering but through class access. Amy Wagers of Harvard, who leads the team that presented the controversial data on GDF11, again presented data during the closing Plenary session at ISSCR 2015. She reiterated that GDF11 was indeed responsible for stimulating the rejuvenation of aged tissue. What was interesting was her resounding affirmation of her previous team’s work with additional clarification of the decrease in aged sampling while postulated the reasons for metabolic interaction. With this new evidence it seems there is a case for continued debate between Novartis and Wager’s group - with the ball now firmly in the big pharma’s court.
Amy Wagers of Harvard, who leads the team that presented the controversial data on GDF11, again presented data during the closing Plenary session at ISSCR 2015. She reiterated that GDF11 was indeed responsible for stimulating the rejuvenation of aged tissue. What was interesting was her resounding affirmation of her previous team’s work with additional clarification of the decrease in aged sampling while postulated the reasons for metabolic interaction. With this new evidence it seems there is a case for continued debate between Novartis and Wager’s group - with the ball now firmly in the big pharma’s court.
Another topic which has been a source of scientific debate, is the efficacy potential of adult MSCs to treat Multiple Sclerosis (“MS”). Much has been written on the potential immunological benefits of MSCs, as well as the therapeutic value in a whole host of degenerative conditions. This potential has to some extent broadened the expectation factor when the reality has yet to be fully materialized in clinical results and approved products with meaningful cost to efficacy ratios. Neuronal diseases are by far the most challenging and a source of patient desperation given they are largely unmet medical conditions - MS being one such disease.
There have been various reports of autologous stem cells being used systemically and directly into the CNS for MS yet none were administered under a FDA approved clinical trial setting and therefore the results, however promising in certain reported cases were not recognized by the community. This therefore makes the situation all the more pressing for validating studies on severe unmet medical conditions - not just in the US but in all territories internationally where stem cell therapies are being applied.
Most recently in Canada they have begun the 1st Canadian MSC trial for MS and the community eagerly awaits the data.
There have been various reports of autologous stem cells being used systemically and directly into the CNS for MS yet none were administered under a FDA approved clinical trial setting and therefore the results, however promising in certain reported cases were not recognized by the community. This therefore makes the situation all the more pressing for validating studies on severe unmet medical conditions - not just in the US but in all territories internationally where stem cell therapies are being applied.
Most recently in Canada they have begun the 1st Canadian MSC trial for MS and the community eagerly awaits the data.
In the US it has largely gone unreported that there is an open FDA approved adult MSC-NP clinical trial at the Tisch School of Medicine in NY with Dr. Violaine Harris & team driving the science and Dr. Saud Sadiq, as the investigator. During the session interim data was presented from 10 patients that had been dosed with 8 to 10m MSCs due to have 3 separate administration sessions. This report was post the 2nd dosing. Safety was shown with mild transient headaches reported (24 to 48 hrs duration). On the effect signal, although it’s still early and only 10 patients, there were no worsening of the disease in any subjects, with 4 showing mild improvement with standing and movement and 3 patients with good improvement. No doubt the full data set will be of interest and it’s a positive sign that under clinical conditions there is a biological effect which may be attributable to the cells. One can postulate that with more potent technology this effect may be accentuated and patients without much recourse will be recruited for larger studies to speed the path forward. Positive presentation.
The last of the three sessions I will relay here is the talk by Mitsutoshi Yamada, a postdoc fellow who works with Dieter Elgi’s at the New York Stem Cell Foundation (“NYSCF”). What I took away from the talk was the viability issue of using screening technology to assist in the process of ensuring safe and effective translation of mitochondrial replacement therapy. It was shown in this study that there was no adverse developmental effects using the NT process, which seemed positive and that there was also solid reporting of integrity analysis. The issue of reported “drift” I believe was tweeted once or twice on the presentation at the time, which was a noted issue requiring follow-up. Paper to be published shortly.
As mitochondrial replacement therapy is being considered in the US and the legal authorization to proceed in the UK allowed it’s fitting that the science investigation continues apace to answer the open questions and look to increase the accumulating knowledge surrounding the technology. Infertility is a curse and a growing problem in today’s stress filled and environmentally polluted world.
As a related aside, I coincidentally stopped at a Poster number looking for a specific study, which I thought would still be up, but which had been taken down and replaced. In its stead was an iPS Egg poster from Taiwan.
I spoke with the investigators and was happy to learn that they are actively pursuing the iPS Egg creation concept for infertility treatment. They relayed that Taiwan has the highest rate of infertility in the world and are near their goal of producing iPS Eggs. I wished them well.
I spoke with the investigators and was happy to learn that they are actively pursuing the iPS Egg creation concept for infertility treatment. They relayed that Taiwan has the highest rate of infertility in the world and are near their goal of producing iPS Eggs. I wished them well.
 This sculpture by my Mother was created some ten years ago for all those women that suffer from infertility - she’s screaming to the heavens…it weighs 500 kilos and was made in Norway of granite - it rests now in the Pyrenees, closer to the sky...
This sculpture by my Mother was created some ten years ago for all those women that suffer from infertility - she’s screaming to the heavens…it weighs 500 kilos and was made in Norway of granite - it rests now in the Pyrenees, closer to the sky...
Cheers
____________________________________________________
The Pluripotency Trilogy
How to unite the themes of varying conversations related to a broad field of study into a summary review is often a challenge, yet when stem cell science is the topic invariably the subject of pluripotency and developmental biology arises as a convenient unifying thread.
 |
| via Nature |
From afar the concepts within the “black box” of cellular processes that define our make-up and function seems highly complex but with the required knowledge of rudimentary electrical circuitry we can all illuminate some shapes of the machine within.
Enter the scientists - no stage door - just straight up the aisle and onto the platform. The scene of all these discoveries is their domain. An often infuriatingly slow and arduous responsibility, willingly accepted, yet obscure mostly to all but those that have the calling to search for the answers amongst the molecules.
Research, I have come to understand and respect, is the very life-blood of the process. For every day spent hunched over the bench, there will be a thousand more, replicated the world over in countless laboratories. The pursuit of knowledge, basic and fundamental, can only be completely appreciated if you are truly a part of that process.
Businesses are built on outcomes. Patients are helped if and only when products have passed the grade. Health systems and government budgets are factors of the efficiencies built into the very fabric of the quality of that basic discovery process.
We rely on research, more than we'd like to admit. The spirit in which the discovery process operates must be preserved, nurtured, funded and importantly bridged so that the world beyond the bench can truly appreciate it’s importance and voice its support.
More so today and tomorrow than perhaps in the past...
The development of therapeutics for clinical application may not be the intent nor goal of basic research and in many ways the practical implications of knowledge inhibits the free expression of intellectual pursuit. This is true of Art also and a number of other fields where creative thought is required or problem solving a key focus.
There are always different perspectives, opinions and methods in every field - no more so than in stem cell science where the factual basis for definitive proof is set high. This perhaps goes to the very heart of the issue - human biological system architecture is still largely an unknown and has evolved over the course of countless millennia. Unravelling the machinations of our inner workings will take time and will require a different set of parameters to assimilate - from all stakeholders.
Onto the protagonists of this story - the scientists - and their take on pluripotency.
I had the opportunity to delve somewhat into the background and focus of three leading scientists attending ISSCR 2015 - Prof. Austin Smith of Cambridge, Jeanne Loring of Scripps and Rudolf Jaenisch of the Whitehead Institute. All three kindly entertained questions on the nature of pluripotency and its importance to the stem cell field.
To set the scene - scientific debate is healthy and an essential component to discovery, as its that essential motivation within the community peer structure that drives insight and translation.
Pluripotency I have come to appreciate is not a clear biological phenomena, as in many ways it’s a transient in-vivo state that when studied outside of the body is an “artificial artefact” as Rudolf Jaenisch termed it.
To provide a little background, all three scientists have a history in studying mouse ES cells, going back 25/30 years or so. This is important to note as the nature and definitions applied to pluripotency, from what I can gather, have arisen out of the original study of mouse embryonic developmental biology.
 Prof. Austin Smith stated focus is in trying to “understand the relationship between stem cells in culture and cells in the embryo, which are not stem cells because they don’t self-renew. So we’re trying to understand how cells that we can grow in the culture dish relate to real developmental entities in the embryo of mice or, of course, ultimately of humans.”
Prof. Austin Smith stated focus is in trying to “understand the relationship between stem cells in culture and cells in the embryo, which are not stem cells because they don’t self-renew. So we’re trying to understand how cells that we can grow in the culture dish relate to real developmental entities in the embryo of mice or, of course, ultimately of humans.”
All agree that “pluripotency” is the capacity or potential to make any cell of the body and germ line. Yet where there is ongoing debate is in the ambiguity of the developmental biology of the various states, the profiles inherent therein, the direct methodologies and the difference between mammalian studies of the mouse versus human cells and the very concept of “embryonic”...
The classic view, if one can call it such at this young stage of the science, which Austin and Rudolf are leading proponents of, is that there is fundamentally a parallel biological mechanism in the relationship between the mouse development process and that of the human.
Rudolf attested to the debate within the community on the “controversy” surrounding the various “pluripotent” states, their expression profiles and the pursuit of “naive” mouse like properties.
These are “interesting scientific questions”, which a number of labs, including Austin & Rudolf’s, are continuing to pursue in the basic research field. Some would say there is a good spirited competition to prove that human cells are or can be made to be equivalent to mouse.
 Jeanne Loring’s view of this is somewhat more pragmatic, having also based her early career in the science on the study of mouse ES cells: “I decided to learn one thing and then move on and learn another and then try to put them together…. I have the mouse ES history, which I share with Austin and Rudolf… human cells don’t act like mouse cells, they’re much harder to grow... whether you can make a human cell with the quality of a mouse” is still being investigated “I just went straight to human pluripotent stem cells and realized they were not going to be like mouse and lived with it… so I just bypassed that… my cells become what I want them to become and that’s it - I’m done.. they don’t need to be mouse cells, they’re human cells”
Jeanne Loring’s view of this is somewhat more pragmatic, having also based her early career in the science on the study of mouse ES cells: “I decided to learn one thing and then move on and learn another and then try to put them together…. I have the mouse ES history, which I share with Austin and Rudolf… human cells don’t act like mouse cells, they’re much harder to grow... whether you can make a human cell with the quality of a mouse” is still being investigated “I just went straight to human pluripotent stem cells and realized they were not going to be like mouse and lived with it… so I just bypassed that… my cells become what I want them to become and that’s it - I’m done.. they don’t need to be mouse cells, they’re human cells”
This internal debate somewhat sheds light on the differences inherent in the basic versus translational aspects of the scientific community. The need for answers and the desire to move forward.
I tried to explore this balance further in the discussions and appreciated that not all science has to be translational, far from it actually, but on the other hand more interconnect perhaps is needed to facilitate translation.
To illustrate Austin and I discussed the issue of pace and method of action - that is we exchanged views on the speed in which scientific discovery is translated and the focus on uncovering the biological roadmap to cellular, molecular and genetics prior to therapeutic treatment of patients in need.
Austin correctly pointed out that “you can’t run before you can walk… and of course from the perspective of a patient or a politician that it seems to be taking an awfully long time… however it is very complex and we have to do it right.” This theme is necessary to broadcast and communicate effectively to the public in a manner which is empathetic to the broader societal issues beyond the lab. There is a need to bridge all perspectives to achieve results.
Further on the topic Austin relayed that “what basic science can contribute is our knowledge & understanding of the mechanisms and of the biology to create a rational approach to therapy…. however, of course you can approach it from the other end, from the clinician’s end which is…. you can try things and you know historically that has been by and large the way medicine has developed and I dare say there will always be a place for that..”
The pure nature of discovery was clearly Austin and Rudolf’s focus, and rightly so - as I said earlier in the article, it is the very life blood of the foundation on which all is built. For more on Austin’s work & views you can read a post ISSCR article here via Development.
I will be featuring more of Jeanne Loring’s interview separately as we discussed her career and projects, including the Parkinson’s iPS work she is progressing at Scripps and also her interesting effort to help the San Diego Zoo with an endangered species via novel fertilization techniques using reprogrammed germ line cells. Stay tuned for that.
It was a pleasure speaking with Austin, Rudolf and Jeanne and I thank them for their time. Their work in the field of discovery and translation are representative of the commitment and intellect devoted to moving the science forward.
I feel like it’s time for cup of tea - I like mint tea, cools you down in the summer… been hovering around 100 degrees here for weeks… off to the beach I think! Enjoy.
Until next week.
Until next week.
Cheers
___________________________________________________________
Jeanne Loring - Parkinson's, Mice, DNA, hPSC & Rhinos

 Jeanne Loring of the Scripps Research Institute in La Jolla California kindly sat down with me at the ISSCR annual meeting for a broad discussion of her history, views on the field and developments in the science.
Jeanne Loring of the Scripps Research Institute in La Jolla California kindly sat down with me at the ISSCR annual meeting for a broad discussion of her history, views on the field and developments in the science.
I found Jeanne a refreshing character, as I did a number of others I was fortunate to met in Sweden. Her style I can only best describe as natural. It must be the Southern California air or something but there is a definite quality of relaxed confidence about her. I liked her a lot and hope to have the opportunity to meet her again sometime - perhaps at the birth of her “to be” Northern White Rhino! If she invites me :) that would be something.
The format of the interview was free flowing and what was clear to me from her long standing scientific focus and deep knowledge of the sector was it takes determination and a varied set of skills to maintain one’s position in today’s fast paced world of cutting edge science and more so even to successfully translate that to the clinic.
Kudos to Jeanne for her efforts to continue the fight to bring forward a therapy for Parkinson's after near on 30 years and for her passion to help our planet’s most endangered.
Hope you find the interview interesting, as much as I enjoyed it.
Cheers
Interview:
M: Tell me a little about your background
 JL: So I was trained in embryology and neurobiology, I studied neural crest cells which are actually stem cells and I was fascinated by them. Then when I finished graduate school I got a job as an assistant professor at the University of California Davis and I then realized I could either teach or do research but not both. There were not enough hours in the day, so I took the opportunity to join a biotech company in California called Hana Biologics. There were lots of them around, in 1987. I joined specifically because they were planning a stem cell therapy for Parkinson’s disease. I thought I could use what I thought was practical because I was getting a little bit tired of generating just knowledge. I wanted to generate practical knowledge which made me a little bit different from everybody else at the time.
JL: So I was trained in embryology and neurobiology, I studied neural crest cells which are actually stem cells and I was fascinated by them. Then when I finished graduate school I got a job as an assistant professor at the University of California Davis and I then realized I could either teach or do research but not both. There were not enough hours in the day, so I took the opportunity to join a biotech company in California called Hana Biologics. There were lots of them around, in 1987. I joined specifically because they were planning a stem cell therapy for Parkinson’s disease. I thought I could use what I thought was practical because I was getting a little bit tired of generating just knowledge. I wanted to generate practical knowledge which made me a little bit different from everybody else at the time.
M: Was that motivated by personal experience?
JL: No I don’t know anybody sick at all it was just I wanted to have more impact than just writing papers. I wanted to do something more important. I probably could have ended up like Rudolf Jaenisch or Austin Smith, in a way, if I was good at it the entire time but when you go into biotech it's guaranteed you'll not be at the same job for more than 5 years. I didn't know that at the time but I've learned now. So the first company I went to work for was doing a cell therapy for Parkinson’s disease but there were no stem cells yet so we were using fetal cells and we were trying to expand them. That was the heyday of the fetal transplants for Parkinson’s disease and it was clear they were working for some people, so why couldn't we take fetal cells and expand them and treat more patients.
M: I attended the pre-meeting symposium @ Karolinska on the aging brain. The eye and brain are related of course but the brain is less accessible.
JL: Yes you just have to pretty much accept that. The eye is accessible therefore it is a good testing ground for therapies. Once you put things in the brain you pretty much don't know what's happened until the person dies.
M: Why did the fetal work not continue?
JL: Yeah I'll tell you, I know exactly why. So there were two groups, sort of areas, there was Andreas Bjorklund of Karolinska/Lund and his offspring who are following in his footsteps and then there were two groups in the US who were funded by the NIH to do clinical trials. I think the people in Sweden will always argue that they had a tremendous success rate. They weren't under the same kind of regulations that were applicable in the US. They had the authority to do this under a physician kind of approval whereas in the US they were required to, or decided to, do a double blind clinical trial. You had to have negatives looking for placebo effects.
M: And surgery?
JL: Yes, I would never do that.
M: Isn't that unethical?
JL: I think it’s unethical now, I would never do it but they were doing it then. They did have the promise of treatment if they didn’t
M: You mean opening them up again?
JL: Yeah, isn't that wonderful, it’s just brain surgery. The people who do brain surgery don't take this issue as seriously as I do, but they know what they're doing. So to continue, the problem maybe 25%/30%, depending on the study, had an adverse effect that was quite dramatic called dyskinesia. So when they got the cells they had Parkinson’s disease, it was treatable with L-Dopa, but then after they had the cells they started having uncontrollable events, like the opposite of that sort of frozen kind of characteristic of people with Parkinson’s disease. They had to be treated separately and it had obviously been caused by the transplant. The question was
M: Why?
JL: Exactly. So the whole thing stopped in about ‘92 perhaps. I remember I was at the society of neuroscience meeting when the results were reported and everyone in the room was saying we can't do this anymore
M: But 75% of the patients...
JL: Were either not helped or they were helped for the rest of their lives and went off drugs. So it was clearly a spectacular therapy.
M: This was so early, late 80s early 90s, wouldn’t you think that with more push in the science
JL: Everything sort of dropped off the map at that stage and people just didn't pursue it anymore.
M: Was it ethically charged?
JL: Yes but the question was do you want to do something to people that had a clear probability of an adverse effect because it's not a life threatening disease
M: It is a debilitating disease
JL: Yes it is a debilitating disease, that’s right. So I know that if you talk to patients they are willing to take that chance.
M: I have a relative that has Parkinson's, in my wife’s family, and it's not just the disease it's what it does to you aside from that. Your whole spinal column changes and that makes everything more painful and difficult.
JL: Everything is more challenging and you know you can never predict whether you’re going to have a good time or bad time today or this morning or afternoon. I know I have a friend that has Parkinson's and he lives in Texas and I talk to him on the phone every once in awhile and it has to be at a particular time of day otherwise I can't understand him at all.
M: Devastating disease, all the neuronal diseases are devastating.
JL: So that was the whole basis for my Parkinson's disease focus and there was a resurgence when stem cells were discovered. Obviously because you can turn them into dopamine neurons or just what you want with quality control.
M: This was the question I had at the brain symposium, why wouldn't you test the neural stem cells themselves as a method of action and let them stimulate the environment.
JL: People have tried that. There was a whole interval where people were trying to treat Parkinson's with cells that were not dopamine neurons and actually it damaged the field because it didn't work. It turned organizations like the Michael J. Fox foundation, an organisation that had supported it, against cell therapy entirely. So they're not funding it now.
M: Were those stem cell originated?
JL: No they were neural stem cells. This was all before pluripotent stem cells. Either adult or fetal derived and those don't make dopamine, they're not dopaminergic neurons.
M: Isn't there a big difference in terms of your understanding of the pluripotent sources in terms of that?
JL: Oh yeah, of course. There’s a huge difference, the cells you get from adult or fetus have not been successfully turned into the same neuronal cell type that dies in Parkinson's. They don't seem to be able to.
M: So what about the pluripotent neural stem cells?
JL: Neural stem cells aren’t pluripotent. I use pluripotent stem cells to make neural stem cells which I then turn into dopamine neurons.
M: Ok
JL: So my next job, because that obviously failed, was to work at a company called GenPharm. This was in the early 90s and I was doing gene knockouts and mouse embryonic stem cells so I got to be at the beginning of one field and the beginning of another field. That company lasted about five years.
M: What technology did you use?
JL: Using homologous recombination which was a brand new idea. Mario Capecchi won a Nobel Prize for it. I like being in the situation where the technology I’m using wins Nobel prizes for people. I kind of think that validates it. We could just about do anything. We could knock-out, we could change genes. This was all pre Crispr-Cas, which is the way people are doing it now. So that was early days for that as well.
I made a lot of mouse embryonic stem cell lines. This was the same time as Austin Smith and Rudolf Jaenisch were using, making and knocking-out genes in mouse embryonic stem cells. That’s where our histories all sort of coincided. We were all around doing this in the early 90s. Although I was at a company. It was a spectacular five years. We did a lot of amazing work. The work I did then is still some of the most highly cited work that I have ever done. It’s amazing, for whatever reason people are still interested in the work we did then. It was really pioneering and it was fun. Then after the company failed I moved on to a company called Incyte Genomics. This was at the peak of the human genome sequencing era, which started around the mid-90s. I worked at Incyte for around 5 or 6 years learning how sequencing worked.
M: Uncovering the map
JL: Yeah and the technology was evolving very fast at that time. So I now had three things - the Parkinsons neural cell transplant idea, stem cells and now genomics/DNA.
M: This all was at the same time as the other groups but your work went unheralded?
JL: The thing if you're going to be heralded you have to stick at one field for a long time and my approach has been to learn something then learn something else and try to put the two things together.
M: and its all coming together now?
JL: It is, everything I've done is coming together now.
M: Tell me about that, because that’s why your back.
JL: Yeah, that's why I’m back, right. Parkinson’s disease - we now have human pluripotent stem cells and I can turn them into dopamine neurons, so all the things that were wrong with the early work I was doing in the late 80s I can now fix. I'm in full control - I can make the cells I want to.
M: Your independent in an academic setting now.
JL: Yeah, I'm an academic with my own lab. That is what I'm directing my lab to do and our areas of expertise. So I have the Parkinson's history and then I have the mouse embryonic stem cell history, which Austin and Rudolf share. You know it’s interesting people who come from a mouse embryonic background and then started working on human ES or iPS cells have been really pissed that the human cells don't act like the mouse cells. They're much harder to grow. So both Rudolf and Austin have been trying, and this is the focus of their lives now, to turn human pluripotent stem cells into cells like the mouse.
M: Is this kind of an internal debate?
JL: Yes whether it’s important or not to do that. Austin & Rudolf are making their careers on this. This is what they're focused on now & intensely competing with each other over whether you can make a human cell with the quality of a mouse cell. That’s because where they grew up from, and for me, also growing up like that, I just went straight to human pluripotent stem cells and realized they were not going to be like mouse and lived with it.
M: Is that because of the quality and body of evidence in the mouse?
JL: Yes, their history with the mouse. The kind of things you can do with the mouse ES cells. They're much more robust than human pluripotent stem cells. Human embryonic stem cells have to be babied, mouse ES cells you can pretty much leave in an incubator and they're fine. So that’s what they missed about it and wanted hESCs to be like that. They’ve actually moved into the direction of trying to make hESCs be like that.
M: To perform better?
JL: Yes, so that then can use all those techniques they used in the mouse and now apply them to human. So I've just bypassed that. My cells become what I want them to becomes and that’s it - I'm done. They don’t need to be mouse cells, they're human cells. To continue, while I was still at Incyte I started a company and derived a whole bunch of hESCs which were on George Bush’s original list.
M: From IVF donations?
JL: Yes, that’s right. I started a company, so I did it in my own company. There were two employees, actually there were 3 employees, as we had a manager. I was the main scientist and I had an assistant.
M: You had a number of lines. What ever happened to those lines?
JL: Well they got acquired by another company and I have no idea, they're probably still in the freezer somewhere. They never did anything with them. Its not important anymore as there are so many lines out here. There are 130 lines or so.
M: And they're sufficient to do the science work?
JL: Yeah, oh yeah. But I don’t work on hESCs anymore. I work on iPS cells because they are equivalent but you can get them from individual people. This is where my genome stuff comes in because I studied and learned all the sequencing and genomic stuff when I was at Incyte, so I had an appreciation and understanding of the methods by which you study the genome of cells, along with all the stuff I learned at different companies.
M: The translational aspect of what you're working on is focused on Parkinson's as a primary program?
JL: Yes there are a lot of reasons for it. The person who came to me with the idea to do a therapy for Parkinson's disease is actually the head of the movement disorders clinic at Scripps Health, which is across the street from me. She thought there ought to be a stem cell therapy for Parkinson's and together we did a bunch of fund raising and we've gotten enough data now. We want to do a personalized therapy, an iPS therapy, and genomics is real important as we want to have quality control
M: This is your approach to it?
JL: Yes one of the things we've learned from studying pluripotent stem cells is that they acquire mutations if they spend a lot of time in culture. So you don't want to put cells with dangerous mutations into people, so that’s where my genomic expertise comes in. Essentially the quality control of the cells we want to transplant.
M: Is that the same risk factor in regard to hESCs?
JL: Yeah they will do the same thing. In fact everything we've done shows to-date that iPS and ES cells are identical and eventually I think that will be accepted. The approach I've taken has been because I worked in genomics and have analysed lots of cell lines not just one.
M: I remember you putting out a paper on this recently that was very exhaustive - 2 years of work
JL: Yeah, 2 years of cell culturing. The scientist I worked with on that is here actually - I'm going to take him to lunch tomorrow. So the whole idea was to try and come up with things that were generalizable to cell lines and different conditions. So almost everything we've done was done on 100s of cell lines so we can come up with general principles instead of for one cell line but for 100s.
M: So if you use 1 cell line that is on the edge of a uniform grouping that will be different than if you select and productize something else within that sequence?
JL: Yes
M: and that’s where we're at?
JL: Yes, right now. Here’s the challenge. If you have different cell lines we know they'll have some diversity. They act a little bit differently, a lot due to the personal genomes of course. These are actually people that have been translated into a culture dish and they'll all act a little bit differently. The challenge we have is to develop technologies and quality control methods to allow us to know how every one of those cells becomes the same thing every single time.
M: Is that a far reaching goal?
JL: I think it's actually going to work pretty well. A lot of this has been developed already. That’s been a high priority all along. Some people think it's never going to work but I don't believe that.
M: Is RNA a part of that process?
JL: Yes absolutely.
M: So the work presented recently by Yamanaka will factor into this.
JL: Yes. So the way we make the cells is important - we’ve investigated that. How you reprogram the cells. The methods we use is harmless to the cells.
M: Is that Sendai?
JL: Yes, that’s right. It turns out we've done whole genome sequencing on a lot of cell lines and we've discovered that it’s benign. The other ones are also benign which is also important to keep in mind.
M: So looking at this from a cost perspective, autologous patient specific treatments are highly personalized but are highly expensive. Is that part of the process strategically?
JL: Yes, that’s right. It’s part of the process. There’s a lot of discussion on personalized therapy and whether it's worth the cost.
M: Of course, if it costs $1 million dollars how many people can actually be treated?
JL: Well, more than you think. It turns out for cancer treatments the amount of money that people are paying is similar.
M: Is this about annuities, is that where we’re going?
JL: No. Somebody needs to figure out how to have insurance reimburse for stuff. Right now we're not worried about that yet. I can see how it’s going to work because the work that’s being done now with T-Cells, this is CAR-T therapeutics they’re calling it.
M: I wrote about that 3 years ago.
JL: There you go. That’s about how much it costs for what I'm doing and yet there are even companies developing this technology.
M: There are many now but there were none before.
JL: Well I remember the first time I heard about it I thought I had no idea you could do that. I didn't know the immune system could do that.
M: The immune system is a powerful force to employ.
JL: Yes it is and that's one of the reasons we’re using autologous therapy. We want the cells to be matched and don't want them to be rejected.
M: Isn't there a movement towards Allogeneic?
JL: It’s hard to say. Yes, probably because of this effort in characterizing cells but let me put it this way. As soon as we demonstrate we can make the same cells from 8 different patients and they all work then the story’s over. Autologous therapy and the price point will be worth it. It will be like CAR-T therapy. It will be what you have to do for the best possible therapy.
M: Wouldn’t you want to test an Allogeneic source?
JL: I don’t want to as others are doing it. I’m going to let them go ahead and do it.
M: and who are those others?
JL: Studer Lab in the US. Actually there’s one other Autologous therapy which is being done in Japan by Jun Takahashi.
M: Coming out next year.
JL: Yeah, his and my project are very similar. We’re trying to collaborate but it’s not going to work I don't think, as it's almost impossible to exchange things between the US and Japan.
M: Really I thought we were friends in many ways.
JL: We are but when it comes to scientific IP, it’s very hard.
M: They do want to license a lot of their underlying technology, Japan Academia, Healios.
JL: and I would be licensing it if I were a company but I don’t have to and that’s another strategy of mine.
M: Don’t they have underlying patents?
JL: Oh yeah and if I decide to commercialize what I develop I’m going to have to license patents from Japan but I'm going to worry about that later. I know a lot about patents too.
M: I remember that.
JL: So therefore I think I have a good strategy. You know the thing is you can never be certain, the science makes sense, the strategy makes sense.
M: To be clear on this patent issue - you don’t need a license to do clinical trials.
JL: No. I don’t need a license to develop anything, as long as I’m an academic and I’m not commercializing it,
M: The concept is Japan Academia is licensing for research purposes because they deliver a package.
JL: Yes - and I don’t need it because I’m a non-profit. They will license their technology for research purposes to companies but they won't let anybody sell the iPS cells. They will just let people generate iPS cells but they charge a lot of money
M: The process of development can happen independently using Sendai without a license.
JL: Yes that’s correct. This is something I know a lot about as I was in biotech and I was affected rather negatively by patents at times. I remember this so clearly I was arguing with one of the WARF patent attorneys, so my friends wanted to challenge the WARF patents. I think we were pretty much challenging for the whole time and the patents finally ran out. They expired just before we lost. The fundamental patents are gone and I challenged the patents because they essentially closed my company. I became an academic, as I like to say to them as many times as I can, so that I would have the freedom to operate and not require a patent from them to do embryonic stem cell research. So as a result of our challenge, very interesting and very educational, we got them to change the claims of their patents. Their fundamental patent on all embryonic stem cells. Originally the wording would have also included iPS cells, so they could have retroactively…
M: There are a few words in there which are specific to embryo derived.
JL: We made them put those in. What happened was we challenged the patents, the patent office rejected all of them, and in order to get the patent office to reinstate them they had to change the language for their primary patent.
M: It was their intent in the first place.
JL: Oh yeah absolutely, that was the strategy but as a result of that they lost any claims to iPS cells so this is a subtle victory and it was a lot of fun. I met some really great people as a result of the patent challenge. The attorney that was with me was the same attorney that brought the challenge to the Myriad patents. He was at the Supreme Court for that and I went to the Supreme Court and got to watch them.
M: Interesting isn’t it
JL: It was fascinating
M: The legal system is a world apart
JL: It’s so bizarre
M: Somewhat like the science world?
JL: No, well in theory yes. What really struck me was the fact that the Supreme Court justices, and I think lay people, need metaphors in order to understand science.
M: They do and communication from science to the world is vital as the boxed view of old school scientists just doing experiments to publish needs to change.
JL: I don’t know why people would do that to tell you the truth.
M: I think there is a value. My curiosity brought me here. So I think there’s a great value in curiosity and the maintenance of that throughout your life
JL: I agree.
M: I like that analogy the Salk Professor, Rusty Gage, presented. He spoke of a running experiment where brain cells develop due to vitality, even in disease states. I’m not sure how a Parkinson's patient can actually get on a treadmill but.
JL: They actually can, this is the cruel thing. Our funding mechanism is patient advocacy based, the people raise money for us.
M: I’m not aware of your funding mechanism.
M: I remember that now - you just recently you did a drive. How did that go?
JL: It’s gotten enough money to get us to the pre-IND stage.
M: Did CIRM ever come in?
JL: CIRM will come through the next round, I believe. We're certainly going to apply for CIRM money. We've been working up to this for a long time. The patients have been going to CIRM meetings so we can educate the panel about the importance of this.
M: How far are you away from the IND
JL: About 2 to 3 years
M: That’s pretty similar to some of the others - Malin Parmer for instance mentioned 2018. Of course the Japanese are coming on fast next year.
JL: They’re on a fast track - there are some positives and negatives about that.
M: Tell me about that. There is I guess a Japanese societal push, an industrial push. They have a tendency to like to do that in industry and it’s been beneficial in the past. Do you see that as a mechanism to dominate?
JL: Oh yes absolutely - that’s why they're doing it.
M: and will it open up things potentially or will there be a downfall?
JL: The good thing as far as I’m concerned, if Jun Takahashi gets his therapy through the regulatory agency, he´ll get to transplant his cells to people and they'll be doing that before I do. It’s quite clear our FDA will not let me do it sooner. So if nothing bad happens to the patients then that will help me. However, if somebody else, because of this fast track, gets on this and there are scientists that are not as careful as Jun Takahashi there could be issues. Stem cell therapy, just like everything else, if it is strongly promoted can have setbacks. In Japan we saw what happened with the STAP problem. As soon as there’s a lot of pressure from the Japanese society and Government to move forward there are going to be people that make mistakes. There will be people that are not careful.
M: Masayo Takahashi is trialing iPS cells.
JL: Yes and she has published preclinical work. Essentially she is trying to show equivalency of iPS to ES cells. I think that´s very important, as the FDA is still very worried about iPS cells.
M: They are it seems. There was some planning to file an IND for Platelets.
JL: Yes.
M: Do you know that story?
JL: I do, yes.
M: Will you tell it?
JL: I probably can. I can publicly say I was a consultant for them [Ocata/ACT] and that I attended their pre-clinical meeting as a consultant. So I know a lot about the reaction of the FDA about that.
M: This was back 3 years ago?
JL: Yeah I think 2 to 3 years
M: 2013
JL: Yeah, and I wasn’t really necessary. I didn't say a word but it was fascinating to see the FDA’s response.
M: The concerns they had were GMP compliance related.
JL: Yes, but they’re getting over that. They’ve approved ES cells which were accidentally made. I mean nobody thought about using them for therapy. So one of the cell lines that they approved was derived in 1998 using bovine serum. They’ve approved something that is far less qualified than the iPS cells we're making now.
M: Yes even the Ocata/ACT cell line comes from some time ago on MEF.
JL: Yeah and I’m not concerned about that. There are some issues with using xeno reagents but they are really related to whether you’re making the cells make the wrong kinds of sugars. That’s essentially all it is. If you were to put mouse embryonic cells or mouse iPS cells on MEF they would get viruses and would be transferred into the cells but since they’re not human viruses they don’t affect human cells. Nobody has ever shown any kind of viral induction.
M: That’s why the safety is intact.
JL: Yeah exactly. Even if that should happen and it doesn’t, you just have to accept that it doesn’t.
M: It’s only a transitory process as well.
JL: Yeah you’re not putting mouse cells into people. But you’re also not infecting the cells so there’s no lasting change.
M: There are a lot of other technologies that are far more dangerous - virus delivery for instance.
JL: Oh yes of course and people are using viruses and they’ve actually been dangerous and demonstrated to be dangerous.
M: There have been a lot of adverse events and people have actually died in the CAR-T trials and no one talks about it.
JL: Yes that’s right.
M: My feeling is the xeno movement is a good thing for standardization and some of the work shown here, the BioLamina work and the Thermo Fisher work, these are very good protocols that need to be adopted and the expansion occur.
JL: That’s fine as long as they are necessary and they work well I don’t really care. I’m not too worried about the xeno issue because the cells won’t be inter species
M: Are they requiring it now, is that the new standard?
JL: Not yet, no. We just had a meeting with our regulatory consultant a couple of weeks ago and of course you never know.
M: So when the Israelis and Biotime and others in the field are touting the xeno-free, it’s just marketing?
JL: I think so, mostly yeah, don’t let's pull it too far, I mean the FDA is never really predictable and they could suddenly think it’s dangerous to have xeno reagents.
M: But the products will be approved without a line switch.
JL: Right, that’s right.
M: What are the programs in the pluripotent space you think will reach the market within the next 5 years?
JL: Obviously there’s a lot of interest in the reagent business and there are a lot of companies that are joining in, especially in Japan. I really didn’t realize how much was involved in Japan in creating reagents for taking the cells to the clinic.
M: ReproCell?
JL: Yeah, ReproCell and there’s this other one.
M: Takara?
JL: Yeah. I’m doing an innovation showcase tomorrow. One of my friends asked me to do it for him because he can’t make it here and it's for another Japanese company. I still have to do my research on them but apparently they’re a very large chemistry company. They’ve been in business a long time and now they want to start to apply what they’ve done to stem cells.
M: Interesting how some of the non-scientific power houses in Japan are involving themselves now. A change in strategy perhaps. Digital is affecting their main lines of business and there’s an opportunity.
JL: Oh yeah, absolutely. They have a lot of bandwidth. Fuji Film just bought Cellular Dynamics. I mean you’re not making film anymore so you might as well make stem cell reagents.
M: I don’t want to press on the point of who’s going to come to market soon but success needs to be translated and your view on early access as being a component of adoption, proof of clinical concept, is that in your view an essential part of regulatory review & language?
JL: Yes, I think so absolutely. I think one of the problems with the way that Japan has fast tracked is that our FDA has not been fully appreciated. I think they’re not going to fully adopt because the Japanese regulatory authorities have decided to trust their scientists a lot more than the FDA trusts us.
M: In my view Japan also has a symbiotic relationship with the other parts of the system, you know, it works all together - the insurance, the legal, the funding, the university/academic and business community.
JL: I know, it’s really amazing. I’m really envious.
M: Anything else on the program front? I wanted to talk about the Zoo work.
JL: I know that’s what you actually wanted to talk to me about.
M: Yes, it was fascinating that you’re doing that work.
JL: Yeah, we decided that we could reprogram endangered species cells so in 2011 we published a paper to say we can - Rhinos, using human technology. That sort of just sat there for awhile.
M: The egg/sperm combination?
JL: All that stuff is coming. At that time we just made iPS cells from the animals and it sort of lay dormant for awhile because the zoo we were working with thought it was a little bit creepy, too Jurassic Park. They've now they decided to embrace it.
M: Weren’t there a number of international groups working on that before?
JL: Yes but not a lot, not in this particular thing. There was a group in Australia that was trying to reprogram other animals.
M: Interestingly in Spain also
JL: Yeah that was different though, replacing one animal with another.
M: Using an animal to host?
 JL: Well they’ve done that too. Yeah, the essence of our approach with endangered animals is to take the pluripotent stem cells and to use the technologies that has been developed for mouse and for humans and make gametes out of the cells. Then use IVF technology, that is also in development for these animals, and have a surrogate host that we’ll be able to put the embryos into and regenerate the species. Just a small thing! I’m doing it with the Northern White Rhino, as there are only 5 of them left. There’s only one male and the females I think, with one exception, are beyond reproductive age and they’re dying.
JL: Well they’ve done that too. Yeah, the essence of our approach with endangered animals is to take the pluripotent stem cells and to use the technologies that has been developed for mouse and for humans and make gametes out of the cells. Then use IVF technology, that is also in development for these animals, and have a surrogate host that we’ll be able to put the embryos into and regenerate the species. Just a small thing! I’m doing it with the Northern White Rhino, as there are only 5 of them left. There’s only one male and the females I think, with one exception, are beyond reproductive age and they’re dying.
M: So how would you approach that?
JL: The Southern White Rhino. It has a very similar reproductive cycle. The Northern White Rhino are a different species but they’re very similar. No one really knows if you can cross them yet, which is kind of interesting as I would have thought they would have figured that out by now but no. So we want to make the gametes from the Northern White Rhino, inseminate the eggs in a culture dish and transfer the embryos to a Southern White Rhino.
M: The egg would come from the endangered species also?
JL: Yes, from the pluripotent stem cells.
M: Both gametes.
JL: Yes both gametes would be produced from iPS technology.
M: Have you proven that yet?
JL: No, we had no money, so we essentially have been generating more iPS cells and we’re getting better at it. But now there’s going to be an investment, that’s what they tell me. The zoo has decided.
M: Which zoo is that?
JL: The San Diego Zoo Wild Park
M: Wonderful.
JL: They’ll be announcing that when they feel like it, it’s not up to me.
M: Very good, I wish you luck with that.
JL: Thanks, it’s one of those things which stuck out.
M: Well worth doing.
JL: Yeah, it is worth doing and it was just a matter of timing. I think a lot of this is like that. If you’re too ahead of people’s understanding of what you’re doing then it will just sit there dormant until they understand it.
M: I think in most fields if you’re pioneering something you have a responsibility to educate.
JL: Yes but people also have to accept it. I’ve seen a lot of changes in the stem cell world since we started this in 1998 so it’s been awhile.
M: The %s are way higher now.
JL: Yeah they're higher, that’s right, and it does have to do with education and our patient advocacy approach means we educate patients and the patients educate other people because they’re motivated. They may have not wanted to be scientists but they’re driven into it because they want to get cured, they want to get treated.
M: Thank you Jeanne
JL: Ok
###
Ref: Parkinson's review by EuroStemCells
___________________________________________________________
Utility by Design - Bio-Engineered MedTech Devices
 I don't believe Dr. Robert Langer needs too much of an introduction. His work and creative mind has motivated some of the brightest scientists to reach forward and look to driving change, as an achievable goal. The Langer Lab at MIT has become synonymous with innovation and a can do attitude. A view that permeates throughout the complex interwoven fabric of chemical constructs, nanoscale architectures and biological systems. This is Bob’s culture, as he likes to be called. Those from yesterday and today all have this in common, as will those of tomorrow - the origin story of innovation without peer. The list is long and distinguished and will be so far into the future.
I don't believe Dr. Robert Langer needs too much of an introduction. His work and creative mind has motivated some of the brightest scientists to reach forward and look to driving change, as an achievable goal. The Langer Lab at MIT has become synonymous with innovation and a can do attitude. A view that permeates throughout the complex interwoven fabric of chemical constructs, nanoscale architectures and biological systems. This is Bob’s culture, as he likes to be called. Those from yesterday and today all have this in common, as will those of tomorrow - the origin story of innovation without peer. The list is long and distinguished and will be so far into the future.
Up until recently that was the realm of dedicated professionals, each with their own areas of expertise. Bob was one of those that looked to change that, perhaps as a result of his requirement to improve what he saw as inefficiencies and his innate ability to bridge between the professional definitions that ordered things. To seek out compatible solutions that mixed disciplines in order arrive at a solution. The utility factor by design. Practical and purposeful from a solutions perspective.
 With the advent of cellular therapy the use and in-vitro manipulation of cell populations has become a common occurrence in laboratories and bio-manufacturing centers around the world. The promise of new biologically relevant patient treatments, both personalized and generic, holds great promise for the medical industry and most of all to patients. Along with the advent of this new era in therapies comes the technologies to optimize and enhance the cell productization process.
With the advent of cellular therapy the use and in-vitro manipulation of cell populations has become a common occurrence in laboratories and bio-manufacturing centers around the world. The promise of new biologically relevant patient treatments, both personalized and generic, holds great promise for the medical industry and most of all to patients. Along with the advent of this new era in therapies comes the technologies to optimize and enhance the cell productization process.
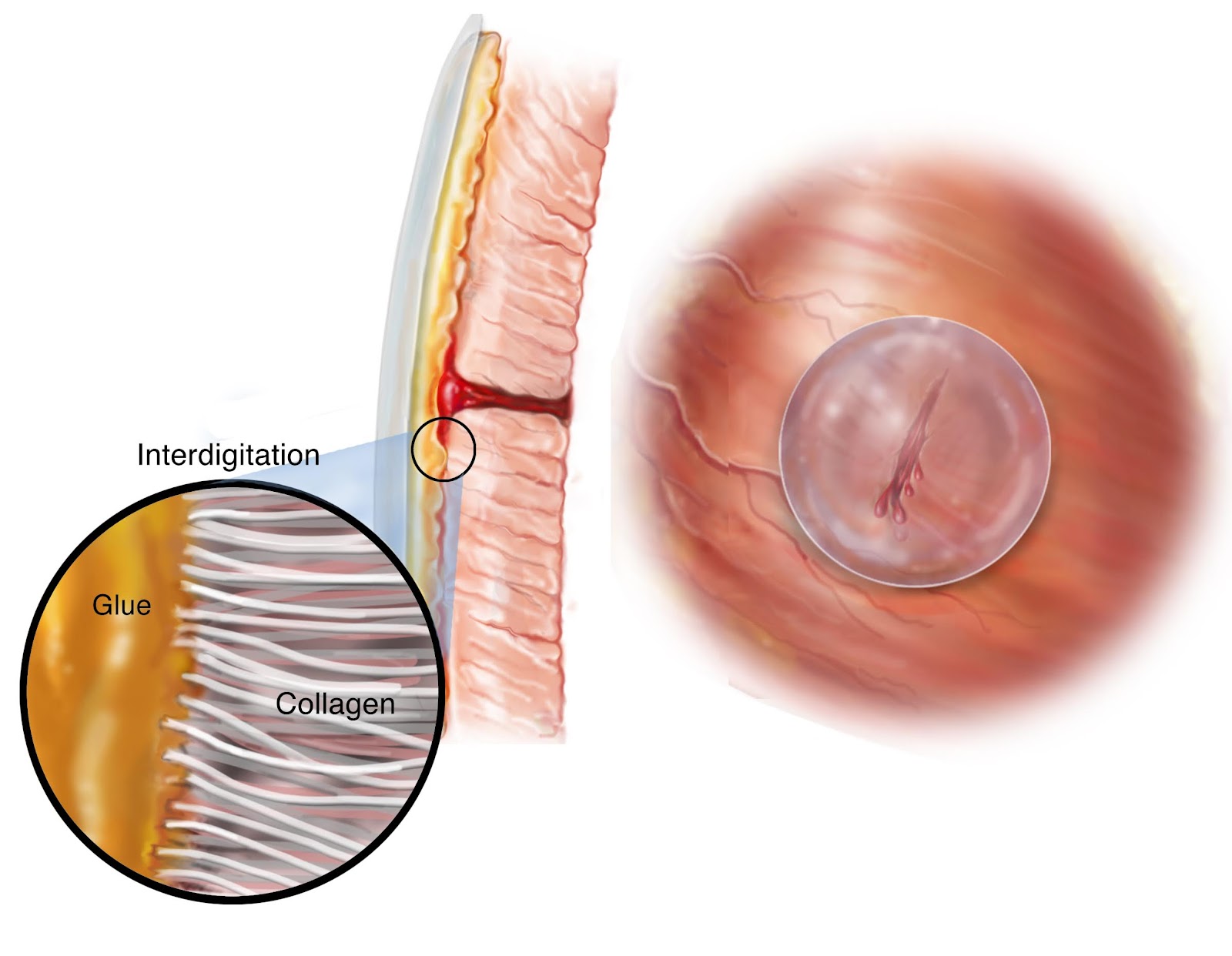 • When we talked to a number of clinicians, they said “There’s certain glues that exist in the clinic that either cure within 1 minute or 10 minutes and we don’t want to be at the mercy of the technology, we want to be in control”; and so we made on-demand adhesion part of our design criteria. We envisioned using light to achieve this.
• When we talked to a number of clinicians, they said “There’s certain glues that exist in the clinic that either cure within 1 minute or 10 minutes and we don’t want to be at the mercy of the technology, we want to be in control”; and so we made on-demand adhesion part of our design criteria. We envisioned using light to achieve this.
 The Neural Stem Cell Institute (NSCI) is home to some of the most interesting work in stem cell technology today. Its origin as a research hub for neural cell investigation lies with Sally's history and her pursuit and discovery of the first CNS stem cells in the mouse. As with a number of other leading scientists she started with uncovering complex neural biological systems and the mechanistic pathways of cell constructs of the CNS, which included the eye. She is the recipient of the MacArthur "Genius" Award and a highly respected leader in the field.
The Neural Stem Cell Institute (NSCI) is home to some of the most interesting work in stem cell technology today. Its origin as a research hub for neural cell investigation lies with Sally's history and her pursuit and discovery of the first CNS stem cells in the mouse. As with a number of other leading scientists she started with uncovering complex neural biological systems and the mechanistic pathways of cell constructs of the CNS, which included the eye. She is the recipient of the MacArthur "Genius" Award and a highly respected leader in the field.
The eye is uniquely interconnected as a sensory organ, yet accessible, which has made it a natural target for NSCI to lead off with. The program is earmarked for a clinical trial in the not too distant future. RPE cell transplants are a hot cell therapy area. A number of groups are in clinical trials using various different sources and application methods using RPEs - notably Ocata, Riken, Coffey/Pfizer & BioTime/CellCure. Some groups are also in the clinic using different retinal cells, while others still are in various pre-clinical stages of development. All this attention and focus on the eye is for a good reason - it's accessible and in-vivo activity can be observed in detail. However, most importantly the momentum is building as the data reported to-date is showing safety & potential efficacy.
Stem Cell Podcast w/ Sally Temple
The adult stem cell discovery that Sally, Jeff and collaborators at their NSCI uncovered has resonated throughout the community. It's simplicity is captivating and it's implications far reaching. The very nature of regeneration and the body's own capacity to heal itself is powerful stuff. That is what we all wish for, methods by which we can assist our own abilities in all manners throughout our lives - why not also with our own health.
 Yet, there is still a basic question to be resolved - if there are these cell populations in our organs & tissue, just waiting for those cues, can we indeed awaken our "Inner Salamander?"
Yet, there is still a basic question to be resolved - if there are these cell populations in our organs & tissue, just waiting for those cues, can we indeed awaken our "Inner Salamander?"
Good luck Sally, Jeff and all the team in my home State!
ST - The idea for discovery research and looking for retinal cells that might have regenerative potential I have to attribute to my husband Jeff Stern. He started in basic research and decided he wanted to work with people and went to medical school. He ended up coming back into the field of ophthalmology but with that research mindset. We of course talked over the years about neural stem cells and the discovery of tissues that you’d think don’t have regenerative potential but actually do.
 ST - Yes, Derek van der Kooy and Vincent Tropepe. In some animals there’s a ciliary margin but it’s not as clear where the ciliary margin is in humans but just in case we removed the anterior portion. We wanted to look within the RPE and we wanted to make sure we knew what cell type we were looking at. We cloned them and made movies of them. We took them from the eye and demonstrated that only a sub-population, less that 10% and in some preparations only 3% of the RPE cells will divide extensively.
ST - Yes, Derek van der Kooy and Vincent Tropepe. In some animals there’s a ciliary margin but it’s not as clear where the ciliary margin is in humans but just in case we removed the anterior portion. We wanted to look within the RPE and we wanted to make sure we knew what cell type we were looking at. We cloned them and made movies of them. We took them from the eye and demonstrated that only a sub-population, less that 10% and in some preparations only 3% of the RPE cells will divide extensively.
 ST - I don’t know if they cloned a single fetal cell. These are adult cells that we cloned out. From a single cell we get a clone and put it in different media conditions and we have shown that the same cell that can give RPE can also produce fat, cartilage and bone.
ST - I don’t know if they cloned a single fetal cell. These are adult cells that we cloned out. From a single cell we get a clone and put it in different media conditions and we have shown that the same cell that can give RPE can also produce fat, cartilage and bone.
 ST - Yes a lot of them. From one donor we can make 5 x 10⁸ cells which is a lot. Let’s say a patient age-related macular degeneration may require 50,000 or 100,000, because you’re only covering that tiny macular region, we hoping one donor’s cells will be able to treat hundreds of patients. We have made plans for all the moving parts. You have to get manufacturing and regulatory to approve so we’re not doing it ourselves. We’re using a facility and transferring the technology so we know they are making the highest quality cells.
ST - Yes a lot of them. From one donor we can make 5 x 10⁸ cells which is a lot. Let’s say a patient age-related macular degeneration may require 50,000 or 100,000, because you’re only covering that tiny macular region, we hoping one donor’s cells will be able to treat hundreds of patients. We have made plans for all the moving parts. You have to get manufacturing and regulatory to approve so we’re not doing it ourselves. We’re using a facility and transferring the technology so we know they are making the highest quality cells.
 ST - It is mostly. It’s funded through the NY State via the NYSTEM program. We wouldn’t have been able to do this without them. They have been tremendous. It’s very expensive. We have got to solve this problem of why it costs so much to do this. They gave us $10.8m over 4 years to do all the preparations for the manufacturing and the efficacy to get to an IND. What we’re hoping once we get through that process is that we can then move into clinical trials.
ST - It is mostly. It’s funded through the NY State via the NYSTEM program. We wouldn’t have been able to do this without them. They have been tremendous. It’s very expensive. We have got to solve this problem of why it costs so much to do this. They gave us $10.8m over 4 years to do all the preparations for the manufacturing and the efficacy to get to an IND. What we’re hoping once we get through that process is that we can then move into clinical trials.
 M - I spoke with Masayo Takahashi the other day, she’s wonderful, and she was explaining how excited her team was about the progressional steps they’re taking from monolayer to suspension. There’s an acknowledgement that there’s a need for suspension in certain cases.
M - I spoke with Masayo Takahashi the other day, she’s wonderful, and she was explaining how excited her team was about the progressional steps they’re taking from monolayer to suspension. There’s an acknowledgement that there’s a need for suspension in certain cases.
 ST - We also grow iPS cells and I think you’re referring to Eyal Banin and Benjamin Rubinoff and the use of NIC. We find it is beneficial yes.
ST - We also grow iPS cells and I think you’re referring to Eyal Banin and Benjamin Rubinoff and the use of NIC. We find it is beneficial yes.
 I don't believe Dr. Robert Langer needs too much of an introduction. His work and creative mind has motivated some of the brightest scientists to reach forward and look to driving change, as an achievable goal. The Langer Lab at MIT has become synonymous with innovation and a can do attitude. A view that permeates throughout the complex interwoven fabric of chemical constructs, nanoscale architectures and biological systems. This is Bob’s culture, as he likes to be called. Those from yesterday and today all have this in common, as will those of tomorrow - the origin story of innovation without peer. The list is long and distinguished and will be so far into the future.
I don't believe Dr. Robert Langer needs too much of an introduction. His work and creative mind has motivated some of the brightest scientists to reach forward and look to driving change, as an achievable goal. The Langer Lab at MIT has become synonymous with innovation and a can do attitude. A view that permeates throughout the complex interwoven fabric of chemical constructs, nanoscale architectures and biological systems. This is Bob’s culture, as he likes to be called. Those from yesterday and today all have this in common, as will those of tomorrow - the origin story of innovation without peer. The list is long and distinguished and will be so far into the future.
The utility of material science as a foundational springboard for patient centric approaches to medical intervention is not novel. There have been devices, tools and technologies throughout the history of patient care. Some of the most important shifts in medical practice has come by way of devices. The hand of the doc always can and should always be assisted with the very best innovations science can develop.
Up until recently that was the realm of dedicated professionals, each with their own areas of expertise. Bob was one of those that looked to change that, perhaps as a result of his requirement to improve what he saw as inefficiencies and his innate ability to bridge between the professional definitions that ordered things. To seek out compatible solutions that mixed disciplines in order arrive at a solution. The utility factor by design. Practical and purposeful from a solutions perspective.
That is what stuck me about Bob during our meeting. His natural ease at distilling a challenge and suggesting a practical pathway to arrive at a solution. Not the only solution, but in most cases a simple solution, which interconnects various synthetic elements to arrive at a bioengineered answer. A product that can work with and within our natural biological systems, often dramatically improving on an existing methodology for the benefit of patient care.
During our conversation we discussed two such technologies that I have been following closely: SQZ Biotech and Gecko BioMedical. In addition, I followed-up with management for further details. Below you'll find a summary of these technologies and the associated Q&A.
A third topic was InVivo Therapeutics, which has been extensively covered by analysts and the media so I’ll only add some color from Bob on the history and developments.
InVivo’s origin story began with a graduate student, Erin Lavik, in the late 90s. She had come to Bob with with her thesis on spinal cord repair as a material scientist student doing her Phd. They talked about creating a scaffold that “looked like the grey and white matter of the spinal cord which we could put neuronal stem cell on.” Erin had been collaborating with Evan Snyder, a stem cell scientist and envisioned a combined biomaterial and stem cell product. The PNAS paper they published with Yang (Ted) Teng, a neurosurgeon, showed “significant improvement in rats” with the scaffold & cell product. Later they showed improvement in monkeys with both scaffold only and to a greater extent with the combined approach with cells. At that time they were approach by Frank Reynolds from MIT Sloan School about Licensing - which launched InVivo. Frank has since stepped down and Mark Perrin now heads the company.
By Bob’s account, “I think Frank and the people at InVivo, thought it best to try to understand things properly, so they started with a scaffold only product. It's also easier from a regulatory standpoint that way.”
By all accounts that decision was correct, as the clinical trial has started and the first three patients have reported improvements.
What no one expected was the first two patients “falling in love & living together - which is amazing!”
Bob says the “long range plans are very exciting, not just for the scaffold but for the scaffold with neuronal cells and possibly the controlled release of different neurotrophic factors, which we’ve done a lot of work on, for the combined product.”
In the meantime there is speculation not only about the source of the neuronal cells, but also about the marriage of Jesi and Jordan, those accidental love birds!
Utility by Design, along with a touch of Karma.
Cheers
SQZ Biotech
 With the advent of cellular therapy the use and in-vitro manipulation of cell populations has become a common occurrence in laboratories and bio-manufacturing centers around the world. The promise of new biologically relevant patient treatments, both personalized and generic, holds great promise for the medical industry and most of all to patients. Along with the advent of this new era in therapies comes the technologies to optimize and enhance the cell productization process.
With the advent of cellular therapy the use and in-vitro manipulation of cell populations has become a common occurrence in laboratories and bio-manufacturing centers around the world. The promise of new biologically relevant patient treatments, both personalized and generic, holds great promise for the medical industry and most of all to patients. Along with the advent of this new era in therapies comes the technologies to optimize and enhance the cell productization process.
SQZ Biotech was born to fulfil that mission and uses it’s CellSqueeze technology to do so.
As a doctoral student in Bob Langer and Klavs Jensen’s labs in Boston, Armon Sharei excelled at the study of microfluidics, the process of passing substances through small chambers to mimic naturally occurring dynamics. During this thesis work Armon discovered that it was possible to alter the integrity of cell walls in such a manner that doorways opened into cells. Bob Langer was as surprised as Armon “when cells went through the device and a little pressure applied the cells would open up and things would go in.” After further study it was revealed that all kinds of molecules etc, large and small, would go in and no harm to the cell was observed afterwards.
After filing patents and publishing the work in PNAS, Scientific America called it one of the world changing ideas of 2014 and the company was launched with institutional & seed support and Armon became its co-founding leader full time.
The company has now secured VC backing to the tune of $5 million and is in industry prototype tests, with a good deal of buzz around the potential.
Certainly the technology has got off to a good start, gaining some traction. Also there is a broad uptake in cell system technologies that can customize and safely adapt therapeutic populations. CellSqueeze could very well be the next step up in the in-vitro cell manipulation suite.
I asked Armon a few questions on the technology -
M: What are the best types of cells to "squeeze" and if there is a most suitable cell type model depending on the payload, i.e. primary types, differentiated cells, size or shape?
A: We have found that the concept works with every mammalian cell type we have tried. To your point, the most promising areas have been primary cells such as immune cells and stem cells which are hard to treat by conventional means but respond very well to our technology. The size and shape of the cells do influence their delivery properties and we have a library of chip designs that accommodate different cells. As for payload, because the delivery process appears to be a largely membrane disruption based process, we can deliver a broad variety of payloads including peptides, proteins, polymers, DNA, RNA, nanoparticles, etc.
M: How would you best describe the squeeze technology and can it be considered a transduction system?
A: We have tended to simply call it a "delivery system" or an "intracellular delivery system". Mostly because transduction tends to be used in the context of viruses and transfection implies nucleic acid delivery.
M: I've noticed a few new systems for delivering payloads into cells - what advantage do you see SQZ having over these other developing technologies? e.g. the UCLA Optofluidics system is looking to do something similar & how do you see these different approaches vis-a-vis SQZ...
A: I think we are going through a period of exciting development in MEMS technologies for intracellular delivery. I have seen reports of many exciting new methods such as nanoneedles, microfluidic electroporation and other physical delivery systems. Ultimately I am most optimistic about our technology because it is robust, simple, and scalable by comparison to other approaches. For example, the nanoneedles can be difficult to fabricate and are not well suited for suspension cells while microfluidic electroporation does not overcome some of the inherent toxicity issues and delivery limitations of conventional electroporation. In contrast, our devices can operate at over 1,000,000 cells/s and have demonstrated applicability to over 25 cell types. Moreover, our papers demonstrate 10-100x greater performance compared to conventional approaches in multiple applications.
M: It has been reported that SQZ is actively engaged in trialing its proprietary system with industry - can you expand a little on that?
A: We have active partnerships with multiple pharmaceutical and biotech companies pursuing applications that are uniquely enabled by SQZ's technology. These often involve delivery of materials that cannot be introduced into cells by conventional means.
M: With your recent capital raise what are your next development steps and timelines?
A: We are accelerating our internal therapeutic programs and developing next generation devices. The company is focused on the development of novel cell therapies using multiple cell/molecular engineering modalities to address acute clinical challenges across indications.
Refs:
- http://www.pnas.org/content/110/6/2082.full?sid=4af1b6ba-7129-40e8-a8ab-ff8fc7b5dd2f
- https://ilp.mit.edu/newsstory.jsp?id=20681
- http://worldwide.espacenet.com/publicationDetails/inpadocPatentFamily?CC=WO&NR=2015023982A1&KC=A1&FT=D&ND=3&date=20150219&DB=EPODOC&locale=en_EP
- http://worldwide.espacenet.com/publicationDetails/inpadocPatentFamily?CC=KR&NR=20140116374A&KC=A&FT=D&ND=3&date=20141002&DB=EPODOC&locale=en_EP
- https://www.bostonglobe.com/business/2015/01/12/genetic-engineering-cheap/A2D1w0Sv6JZXb7UDiEmqQI/story.html#
- http://newsoffice.mit.edu/2015/cell-squeezing-device-vaccines-0522
- http://newsroom.ucla.edu/releases/ucla-researchers-deliver-large-particles-into-cells-at-high-speed
Gecko Biomedical
As the name inspires, Gecko is a product of nature, developed as a mechanistic solution to the closure and repair of tissue in wet conditions.
As I recall, I was drawn to this technology as a result of my father’s experience as a surgeon and his constant struggle with closure and repair. From his days as a field surgeon in Vietnam to his surgery days at the hospital, he always wished there were more effective closure tools so he could perform better. Occasionally I would listen to him speak about those young soldiers.
The need is real and the solution a potential breakthrough. To be able to close an internal or external wound with the ease and elegance of a bio-patch is a proactive step forward.
Langer again was instrumental in providing the fertile ground, this time for post-doc Jeff Karp, now an Associate Professor at Brigham and Women’s Hospital, Harvard Medical School. As Langer relayed, Jeff loved “to take things out of nature and make them into synthetic materials and one day we were talking about Geckos and if we could make a polymer similar to a Gecko’s grip and we did by nano-printing.” That was the start of development and since then the technology has evolved with advanced glue inspired by snails & worms, along with the integration of light activation chemistry.
Gecko Biomedical is based in Paris and concluded a successful private placement with VCs for $11m, and is running preclinical studies in preparation for first in human trials later this year. Another Langer venture, Moderna, a mRNA company, was the catalyst for the French connection, as he was introduced to Gecko’s future management via Moderna’s executive suite.
I asked Jeff Karp for a little background on the technology and its applications.
M: Can you explain a little about the product solution
J: There is a huge unmet need for better tissue adhesives. Sutures are extremely time consuming as with each pass of the suture needle, the tissue needs to be re-aligned. And the longer a patient is on the operating table the greater the chance for complications. It is also difficult to tie knots in small spaces, such as during laparoscopic procedures. Staples are also problematic as anytime one pushes a staple into tissue, the hole that is created is larger than the staple which tears the tissue, and this can serve as a nidus for bacterial infiltration. And typically you need to bend staples to secure them in place which damages the tissue. Often staple tracks are sites of infection! Also it is challenging to apply staples in small spaces as the devices used can be quite bulky. And sutures and staples have different properties than tissue and this mismatch can cause tissue death over time and lead to leaks.
M: How did you develop the design requirement for the platform
J: We put together a design criteria for the solution -
• We wanted this to work in the harshest environment inside the body, inside a beating heart; it is a highly dynamic environment, it’s very wet, lots of proteins. Many of the glues that exist today that are being used for tissues can become fouled in the presence of blood. As soon as they contact blood they can no longer adhere to tissue so we had to solve that problem.
• We wanted it to be degradable and Biocompatible. What I mean by this is because we are trying to treat kids, we wanted this to facilitate the migration of cells overtop and into it so as the material degrades, it would be replaced with the patient’s own tissue. So at the end of the day, maybe 4 months or 6 months, you’d just be left with the patient’s tissue and that can grow overtime so you don’t have to come in and do revision surgeries.
• It needed to be elastic as the heart is undergoing multiple expansion/contraction cycles.
• Also, we wanted this to resist washout in the heart which is very challenging because there is a high shear stress.
• We had materials that could address many of these, but not washout & adhesion. We couldn’t figure out a way around it so we turned to nature for inspiration and we synthesized glue inspired by slugs snail and sand castle worms. We produced a viscous prepolymer, that you would apply to the tissue or to a patch and then cure with light to end up with a material that’s very similar to an elastic band. We made this patch you can stretch it over and over again but it’s fully degradable and biocompatible. It can take a 30% strain, which is what you’d expect in the heart, and we don’t see much change in the mechanical properties of the material. Eventually we showed that we could seal the carotid artery and aorta of a pig, and also attach a patch inside a beating pig heart.
I also asked Christophe Bancel, CEO of Gecko Biomedical, a few questions on the formation of Gecko and the technology platform moving forward.
C: Bernard Gilly (Non-Executive Chairman) and I knew Bob and Jeff Karp and their the work in the field of adhesives in wet and complex environment for a certain time and we followed their progress. Once the 4 of us believed that the technology was ready to start translation into a product, we decided to create Gecko Biomedical.
M: Why Paris and not the US?
C: From a regulatory and development point of view, many innovations in Medtech tend to be developed in Europe first, so we thought that this could be an opportunity. On top of that, Bernard had developed an entrepreneur initiative in Paris, the iBionext Network, that had successfully brought together experienced executives in Biotech and Medtech with support of leading European investors. We were ready to provide the full support for the development of this technology into innovative products for patients.
M: How do you view the underlying technology
C: Gecko Biomedical’ platform allows the development of diverse solutions for adhesion and wound closure in wet and complex environment that can be designed to meet the requirement of specific tissues. Applications range in the different fields of surgery. We have decided to start focusing on vascular reconstruction, but are also developing variants of our polymers for new tissue types.
M: Will there a combined product with biologics in a future generation of products?
C: Indeed, by design, our family of polymers can provide controlled release of active substances (small molecules or biologics) and also encapsulate cells for active delivery.
M: Where are you at present in the product development timeline?
C: Currently we are working with a leading cardiovascular department at Paris Hospital. We are finalising all the regulatory development under Good Laboratory Practice (GLP) for the non-clinical validation of our first application in vascular reconstruction and intend to start the first clinical trial by year end.
Refs:
- http://www.geckobiomedical.com/
- http://www.nature.com/news/barbs-make-porcupine-quills-into-nasty-needles-1.11986
- http://phenomena.nationalgeographic.com/2012/12/11/why-porcupine-quills-slide-in-with-ease-but-come-out-with-difficulty-2/
- http://www.the-scientist.com/?articles.view/articleNo/36093/title/Sticking-Power/
- http://phenomena.nationalgeographic.com/2013/04/16/parasitic-worm-inspires-better-sticky-medical-tape/
___________________________________________________________
Sally Temple - Cells, Leadership & Audacious Innovation
The eye is often referred to as the window into the soul. Whether that is true or not depends I suppose on who’s doing the viewing, as the subjective interpretation invariably dictates the meaning. This however in science can be balanced via rigorous protocols of evidence based assessment in a clinical setting and peer review. The subjective becomes objective and the perspective become clearer.
In the stem cell field some of the earliest approaches to regenerative medicine have been in the CNS, with a number of high profile clinical stage multi and pluripotent trials. Those in the clinic with ongoing trials are reporting promising indications of disease stability and restorative potential. More data is required but the overall momentum moving forward portends to a variety of treatment methodologies from a number of cell sources. An active area of CNS clinical research has been for the retina, where there are unmet medical conditions in need of new effective solutions for low vision & blinding diseases. Early attempts to restore retinal function via the transplantation of donated adult and fetal retinal tissue and cells were deemed inefficient and lacked solid efficacy data. Those experiments however have paved the way for the current focus on using more developed & novel multipotent cells, as well as from pluripotent sources. One such retinal program is being led by Dr. Sally Temple of the Neural Stem Cell Institute based on a unique population of adult retinal stem cells. I sat down with Sally at ISSCR 2015 and it's fitting she rounds out the Interview segments from Sweden as she is ISSCR's President Elect now and is looking to the future, as we all are, with high expectations and great promise to meet those tangible opportunities head on.
In the stem cell field some of the earliest approaches to regenerative medicine have been in the CNS, with a number of high profile clinical stage multi and pluripotent trials. Those in the clinic with ongoing trials are reporting promising indications of disease stability and restorative potential. More data is required but the overall momentum moving forward portends to a variety of treatment methodologies from a number of cell sources. An active area of CNS clinical research has been for the retina, where there are unmet medical conditions in need of new effective solutions for low vision & blinding diseases. Early attempts to restore retinal function via the transplantation of donated adult and fetal retinal tissue and cells were deemed inefficient and lacked solid efficacy data. Those experiments however have paved the way for the current focus on using more developed & novel multipotent cells, as well as from pluripotent sources. One such retinal program is being led by Dr. Sally Temple of the Neural Stem Cell Institute based on a unique population of adult retinal stem cells. I sat down with Sally at ISSCR 2015 and it's fitting she rounds out the Interview segments from Sweden as she is ISSCR's President Elect now and is looking to the future, as we all are, with high expectations and great promise to meet those tangible opportunities head on.
 The Neural Stem Cell Institute (NSCI) is home to some of the most interesting work in stem cell technology today. Its origin as a research hub for neural cell investigation lies with Sally's history and her pursuit and discovery of the first CNS stem cells in the mouse. As with a number of other leading scientists she started with uncovering complex neural biological systems and the mechanistic pathways of cell constructs of the CNS, which included the eye. She is the recipient of the MacArthur "Genius" Award and a highly respected leader in the field.
The Neural Stem Cell Institute (NSCI) is home to some of the most interesting work in stem cell technology today. Its origin as a research hub for neural cell investigation lies with Sally's history and her pursuit and discovery of the first CNS stem cells in the mouse. As with a number of other leading scientists she started with uncovering complex neural biological systems and the mechanistic pathways of cell constructs of the CNS, which included the eye. She is the recipient of the MacArthur "Genius" Award and a highly respected leader in the field.
NSCI is funded by the NY State NYSTEM along with donations as a non-profit and is based in upstate NY - near Albany, in a town called Rensselaer. It holds a foundational patent estate to an adult stem cell discovery that now forms the lead translational focus of the institute - an adult retinal stem cell in the RPE layer which can be sourced from donor tissue and expanded to therapeutic doses. This same cell can also form a variety of other cell types via a biological trans-differentiation pathway called the EMT into bone, fat and cartilage. The team has published a number of high profile papers (eg 1,2,3) on the science which underpin the clinical translation work. Their projects have many prestigious collaborators, including the Kellogg Eye Center and Mount Sinai, amongst others.
The eye is uniquely interconnected as a sensory organ, yet accessible, which has made it a natural target for NSCI to lead off with. The program is earmarked for a clinical trial in the not too distant future. RPE cell transplants are a hot cell therapy area. A number of groups are in clinical trials using various different sources and application methods using RPEs - notably Ocata, Riken, Coffey/Pfizer & BioTime/CellCure. Some groups are also in the clinic using different retinal cells, while others still are in various pre-clinical stages of development. All this attention and focus on the eye is for a good reason - it's accessible and in-vivo activity can be observed in detail. However, most importantly the momentum is building as the data reported to-date is showing safety & potential efficacy.
Sally's team at NSCI includes her co-founder & partner Jeffrey Stern, a retinal surgeon, and a notable listing of well respected scientists and researchers, including: Chris Fasano, a leading member of the investigator team, who is also known for producing the official ISSCR Stem Cell Podcast with Yosif Ganat.
The work at the institute is not solely eye cell centric, as you will see when exploring the various sub-sections of the research going on there. The basic theme throughout is indeed neural and CNS in general.
Stem Cell Podcast w/ Sally Temple
The adult stem cell discovery that Sally, Jeff and collaborators at their NSCI uncovered has resonated throughout the community. It's simplicity is captivating and it's implications far reaching. The very nature of regeneration and the body's own capacity to heal itself is powerful stuff. That is what we all wish for, methods by which we can assist our own abilities in all manners throughout our lives - why not also with our own health.
 Yet, there is still a basic question to be resolved - if there are these cell populations in our organs & tissue, just waiting for those cues, can we indeed awaken our "Inner Salamander?"
Yet, there is still a basic question to be resolved - if there are these cell populations in our organs & tissue, just waiting for those cues, can we indeed awaken our "Inner Salamander?"
I hope you find the interview transcript below informative. I have great admiration for innovators and no more so that those that fight for patient solutions in a not-for-profit foundation.
Good luck Sally, Jeff and all the team in my home State!
Cheers
Interview
M - Can you explain your discovery of an adult retinal stem cell and use of that for research and therapeutics.
ST - The idea for discovery research and looking for retinal cells that might have regenerative potential I have to attribute to my husband Jeff Stern. He started in basic research and decided he wanted to work with people and went to medical school. He ended up coming back into the field of ophthalmology but with that research mindset. We of course talked over the years about neural stem cells and the discovery of tissues that you’d think don’t have regenerative potential but actually do.
M - Stimulated to have that potential?
ST - That’s the point. I firmly believe that we have that ability and if we can simulate it we can.
M - Somewhat like the salamander effect?
ST - Exactly. So Jeff put in recently for the Audacious Goals competition of the National Eye Institute. All the applications were anonymous so no one knew who submitted what and it was open to everyone, worldwide. They picked 10 winners and one of those was Jeff’s project. He was picked for “Reawakening your Inner Salamander” to take advantage of that.
M - I like it. I used a salamander image a little while ago - it’s a poignant reference.
ST . It is and of course the salamander RPE can regenerate and make the entire neural retina. So if you remove the photoreceptors and you remove the neural retina entirely in salamanders the RPE cells will change, proliferate and then make new retina cells.
M - Was this an area of study for you and your husband?
ST - We were aware of that because when Jeff worked in vision doing physiology, the physics of electrical physiology, he worked with salamanders and so he was very familiar with the regenerative literature and we thought let’s look in the human eye for a stem cell and if so could it be activated. We did experiments to establish these stem cells in the human system. We grew them in clones so we could watch an individual cell and see how many progeny it could make.
M - From what source?
ST - We took it from human cadaver tissue and we removed the retina and took the RPE, which you could obtain very cleanly. We removed the anterior portion of the eye, which people have said may contain proliferative cells in perhaps a ciliary margin.
M - The Canadians?
 ST - Yes, Derek van der Kooy and Vincent Tropepe. In some animals there’s a ciliary margin but it’s not as clear where the ciliary margin is in humans but just in case we removed the anterior portion. We wanted to look within the RPE and we wanted to make sure we knew what cell type we were looking at. We cloned them and made movies of them. We took them from the eye and demonstrated that only a sub-population, less that 10% and in some preparations only 3% of the RPE cells will divide extensively.
ST - Yes, Derek van der Kooy and Vincent Tropepe. In some animals there’s a ciliary margin but it’s not as clear where the ciliary margin is in humans but just in case we removed the anterior portion. We wanted to look within the RPE and we wanted to make sure we knew what cell type we were looking at. We cloned them and made movies of them. We took them from the eye and demonstrated that only a sub-population, less that 10% and in some preparations only 3% of the RPE cells will divide extensively.
M - Do you believe in-vivo they do that on a regular basis or are they stopped?
 |
| VPR - Fibroblastic Scar (UCL image) |
ST - In-vivo people have found it very hard to see any proliferative cells but there are circumstances in which the RPE is thought to proliferate. Unfortunately under certain pathological circumstances you will see the RPE layer migrate through the retina and out into the vitreous and proliferate through creating these awful contractile membranes which will pull the retina off. That type of epiretinal membrane formation is quite common.
M - Almost like a mutated cell process.
ST - It’s like some of the cells are undergoing some of the transformative processes of the EMT state. So we knew there were circumstances under which some of the RPE can proliferate in-vivo. Perhaps sometimes this can be beneficial. Maybe they could proliferate a little bit and help the retina recover from damage.
M - They already do a lot of work.
ST - Yes, the RPE are amazing. They’re such a humble little cell but if they die the retina dies. That’s how important they are. They are important for the blood retina barrier, fluid balance, cytokine protection, phagocytosis and more. So we found a sub-population of the cells will self-renew extensively making hundreds and thousands of cell progeny from one cell.
[discussion break]
M - To recap there are adult retina cells that can proliferate as evidenced by the EMT phenomena and that if stimulated can be a source of retinal tissue
ST - Exactly, so the idea is there’s a sub-population that can be activated to proliferate. If those are the cells that contribute to those abnormal masses we don’t know for sure but what we do know is that the cells can proliferate. We can take a single cell and make numerous progeny. We can split those prodigy up so now we have clones of those originals that you can then put in different media.
M - More so than what was achieved with fetal cells?
 ST - I don’t know if they cloned a single fetal cell. These are adult cells that we cloned out. From a single cell we get a clone and put it in different media conditions and we have shown that the same cell that can give RPE can also produce fat, cartilage and bone.
ST - I don’t know if they cloned a single fetal cell. These are adult cells that we cloned out. From a single cell we get a clone and put it in different media conditions and we have shown that the same cell that can give RPE can also produce fat, cartilage and bone.
M - Along the MSC line?
ST - Yes so RPE can make MSCs and can undergo EMT. We think that could be a good model for the epiretinal formation. We don’t know if it’s the originating cell in-vivo but it can do that. It was a surprise because you wouldn’t have thought of a CNS cell giving rise to MSC progeny.
M - I’ve spoken with Dr. Maher in Barcelona who is pioneering a lot of work on wisdom teeth and he says the same thing in reverse. They can make neural crest cells and other non-MSC cell types, plus the MSC lineages . Does this have to do with the CNS connection also?
ST - The CNS is the brain, the retina and the spinal cord. The neural crest of course is from the dorsal part of the neural tube and its migratory. The cranial neural crest does have progenitors that give rise to bone and cartilage etc. A mixture of cells, as well as neural cells. We know that our cells are CNS cells at the beginning and are probably not going through the neural crest stage. They don’t seem to make sensory neurons and sympathetic neurons etc. We don’t think of changing RPE into neural crest. For some reason the RPE has retained the potential to make MSCs for whatever reason. I can’t explain but that is the case.
M - Have you done genetics on that?
ST - Yes we’re in the process of doing that now and studying this progression into MSCs because we want to understand that so we can prevent, but that happens pathologically. At the same time we know we can take those cells and make beautifully stable RPEs for 2 years in culture.
M - and make a lot of them
 ST - Yes a lot of them. From one donor we can make 5 x 10⁸ cells which is a lot. Let’s say a patient age-related macular degeneration may require 50,000 or 100,000, because you’re only covering that tiny macular region, we hoping one donor’s cells will be able to treat hundreds of patients. We have made plans for all the moving parts. You have to get manufacturing and regulatory to approve so we’re not doing it ourselves. We’re using a facility and transferring the technology so we know they are making the highest quality cells.
ST - Yes a lot of them. From one donor we can make 5 x 10⁸ cells which is a lot. Let’s say a patient age-related macular degeneration may require 50,000 or 100,000, because you’re only covering that tiny macular region, we hoping one donor’s cells will be able to treat hundreds of patients. We have made plans for all the moving parts. You have to get manufacturing and regulatory to approve so we’re not doing it ourselves. We’re using a facility and transferring the technology so we know they are making the highest quality cells.
M - This is an academic institution?
ST - Yes it is. An academic GMP facility at the University of Rochester and they’ve been wonderful. We do a lot of back and forth to make sure the cells are correct.
M - This is sort of a NY project?
 ST - It is mostly. It’s funded through the NY State via the NYSTEM program. We wouldn’t have been able to do this without them. They have been tremendous. It’s very expensive. We have got to solve this problem of why it costs so much to do this. They gave us $10.8m over 4 years to do all the preparations for the manufacturing and the efficacy to get to an IND. What we’re hoping once we get through that process is that we can then move into clinical trials.
ST - It is mostly. It’s funded through the NY State via the NYSTEM program. We wouldn’t have been able to do this without them. They have been tremendous. It’s very expensive. We have got to solve this problem of why it costs so much to do this. They gave us $10.8m over 4 years to do all the preparations for the manufacturing and the efficacy to get to an IND. What we’re hoping once we get through that process is that we can then move into clinical trials.
M - If you can show there’s a signal. I’m not sure if you’ll need to go through a small trial to get to that stage.
ST - Probably a Phase 1. We’re planning about 18 patients. It’s very interesting to be in an area like this. In the beginning people weren’t talking very much about the RPE and then there was a recognition that this would be a great target tissue because it’s the eye and you can actually watch what’s happening once you put the cells in. There are sensitive visual tests.
M - Have you added all those specialists to the team now?
ST - Yes. Jeff of course is a retinal surgeon.
M - Will he be part of the trial?
ST - We think it’s important to be hands off with the safety study, so it will be done independently. That way we have some comfort. We’ll know the cells are safe and there will be no conflict.
M - Once you publish you can receive credit.
ST - The efficacy data to-date is really exciting.
M - Using the RCS rats?
ST - Yes, the RCS rat. You know people have said with that model anything works. This is not true.
M - You can look at the past examples
ST - We haven’t published yet but what we have shown is that the cells have to be at a particular stage of development.
M - That’s what I’ve been talking about before and with the community here.
M - Yes that’s right Robin Ali’s work and clinically with Dr. Lanza’s trials having used cells differentiated to a certain point.
ST - There’s a sweet spot in the developmental profile - the earliest proliferating cells and the latest mature cells don’t work as well as cells in the middle of the process.
M - Yes. It’s important to get there as efficiently as possible, extract, freeze & thaw?
ST - Yes. That sweet spot was a surprise so we’re lining up all these elements to use the cells. I do feel good now having different groups using different sources. Some using iPS, some using ES some putting them on a scaffold and some injecting a suspension - like we plan to do.
 M - I spoke with Masayo Takahashi the other day, she’s wonderful, and she was explaining how excited her team was about the progressional steps they’re taking from monolayer to suspension. There’s an acknowledgement that there’s a need for suspension in certain cases.
M - I spoke with Masayo Takahashi the other day, she’s wonderful, and she was explaining how excited her team was about the progressional steps they’re taking from monolayer to suspension. There’s an acknowledgement that there’s a need for suspension in certain cases.
ST - Oh good. I’m glad she’s doing that.
M - That was very important to hear as I felt there was the advanced stage but there are of course other stages. Robin Ali felt that photoreceptors need to come into play more and importantly so as to restore function & vision. That’s certainly true depending on the disease, state of the eye and point in time. The patient acceptance of surgery along that progression is vital to understand because if you’re looking at 20/40 or 20/80 you're going to have a different opinion than if you were 20/200+ so there is an issue there imo.
ST - So Jeff, if he was here, he would say to you “I’m a retinal surgeon and if there was a non-surgical solution I would prefer it.” That’s why we’re excited by the cell we’ve identified as it’s in our eyes. The RPE is so neat, it’s actually laid down in the embryo so when we look at the eye it’s the black center. Those cells were done when you were in utero and really don’t proliferate very much. So we think that’s one of the reasons we’ve been able to activate them from even a 99 year old. They haven’t been used up. There’s no hayflick limit as they haven’t been dividing and dividing and exhausted. They have preserved their potential to divide. We take them out and put them in culture. These cells from 99 year olds that have not divided for a century will start to divide in 36 hours.
M - Source therefore is not that big an issue for you. Is it the standardization in the manufacturing area that will be a challenge?
ST - Not really, cadaver eyes are readily available because they are already collected for corneal transplants
M - The donor consent forms are already there.
ST - Yes. People are so wonderful in their generosity because these are light & vision saving possibilities. So the cornea is already taken, we take the part that is generally thrown away and utilize that. They’re available and they’re in us. So if they’re there and we could activate them safely for an endogenous repair that would be the goal.
M - Have you seen the BMP4 inhibition study from Derek van der Kooy’s team? He was trying to do something similar. Evidentially there was some form of stop in his cells also and they’re working to find some chemical formula to regulate inhibition but you have to be very specific otherwise they show off target effects.
ST - The RPE cells in-vivo don’t divide very much, if at all, the question is whether this is because of inhibition or the lack of activators. So what we found is we can take growth factors that stimulate the growth in-vitro and put those in the eye of animals and they do activate the cells. We think lack of activators is probably one of the reasons and we can add these. At the same time it’s possible that if you add in something that Derek is describing you get even more activation but I think you have to be very careful. You don’t want too much activation because there would be a concern there you could get a growth.
M - jCyte are doing some interesting work. They’re looking at delivering the factors by way of cells intravitreally.
ST - Yes we’re looking to actually isolate the factors
M - CIRM has funded their program. Henry Klassen is moving it and they’ve got an approved IND for RP [since this interview clinical trial has started - see here].
ST - Yes he’s putting cells in to protect
M - He experimented on different formats and settled on the cells as factor delivery vehicles as his approach first
ST - Good idea
M - There are other possibilities for action via MSCs intravitreally or systemically plus via some of the recent work on neuroprotection using photoreceptor progenitor factors. Is that something similar in how it may work?
ST - Perhaps. I know that Jensen are putting umbilical cord cells under the retina
M - They haven’t been too revealing in terms of data
ST - Right, that’s something I would say is so helpful if we’re working in the same area to share as much as possible because we learn from each other. I don’t know what they’re doing and it’s a highly sensitive area of the body, so safety is a key issue. So to have to inject subretinally once may be ok, but to have to do it repeatedly is a concern. Certainly if you could do an intravitreal injection of an activating factor that has great appeal.
M - Is that where you’d like to get to
ST - Yes. Our animal studies in that area are progressing. We think we have a pipeline developing
M - So the first would be the transplant then during that phase you would develop the concept further?
ST - Yes the endogenous stimulation that’s exactly what we’re doing
M - That’s a plan that will be successful imo - the degree of success is yet to be seen of course but it’s worth every effort.
ST - Of course
M - I noticed you were working with the Israelis on an element of the protocols using NIC expansion. Are you utilizing some of that methodology?
 ST - We also grow iPS cells and I think you’re referring to Eyal Banin and Benjamin Rubinoff and the use of NIC. We find it is beneficial yes.
ST - We also grow iPS cells and I think you’re referring to Eyal Banin and Benjamin Rubinoff and the use of NIC. We find it is beneficial yes.
M - It helps with proliferation or how?
ST - Not quite sure what it does to the cells but it helps the differentiation of the cells and they look robust.
M - Do they over mature as a result?
ST - I don’t think so
M - Ok there’s a sweet spot issue that’s important
ST - Yes so that is the case for our adult cells, which I mentioned we’re preparing a paper on.
M - When’s that due out?
ST - Oh yes, I think Richard Davis, who’s working with us on that, would say “ah, the figures are almost all done, writing it up”
M - In the post!
ST - I know, it’s in the post! I’ll will let you know when it’s ready.
M - Thx, would love to read it. I think we’ve covered so much, just a few more notes here. The Allo source, is there a need for immunosuppressants - systemic or local dose? How will that work?
ST - I have to say when doing a clinical trial you have less leeway than you’d imagine on these different details. We’ve been encouraged to do a very strong immunosuppression early on and part of our clinical team includes physicians that specialize in immune issues in the eye. A uveitis specialist. We recruited a very prominent scientist at Mount Sinai, his name is Douglas Jabs. So we’re aware of that. Because the RPE is the blood retina barrier if it is diseased you could get it broken down. So we’re starting with Allo and the tissue is prevalent and available enough that we could HLA match to help reduce the immune issue. Then, given the cells are already in the eye, if the activation product doesn’t work we could probably do an extraction & expansion for an autologous transplant of cells.
M - Would you do an iPS or a retina stem cell sample from the eye?
ST - We’d probably take it directly from the eye
M - Because a skin biopsy or blood sample is easier
ST - It is. We also know we can take these cells from the subretinal fluid. They’re there and it’s probably just going into the subretinal space and sucking some out. The reason we know this is that in certain circumstances they have to take out fluid such as in a retinal detachment and normally that is thrown away. We have a protocol to grow cells from that. It’s small scale and it doesn’t work every time but we’re not actively trying to harvest the cells right now, but in theory it could be done.
M - I’m very happy for you and your team - it’s great work. At the end of the day fighting hard for the future solutions is really all about the next generation and what we can do for our own loved ones who are older. If we can stop this evil circle it will be worth it and try to do it in a way that makes it economically viable. Thank you so much Sally.
ST - Thank you.
Refs:
- Adult Human RPE Can Be Activated into a Multipotent Stem Cell that Produces Mesenchymal Derivatives
- Untapping the Potential of Human Retinal Pigmented Epithelial Cells
- The culture and maintenance of functional retinal pigment epithelial monolayers from adult human eye
- Human RPE Stem Cells Grown into Polarized RPE Monolayers on a Polyester Matrix Are Maintained after Grafting into Rabbit Subretinal Space
- RPESCs Patent - US Grant July 2013
- RPESC Patent Family - EspaceNet
- Related Program IP



































